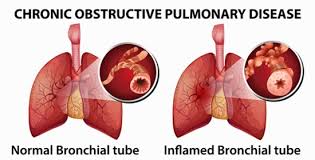
Chronic bronchitis, defined as a productive cough lasting for at least three months over two consecutive years, often results from persistent inflammation and microbial colonization of the airways. Among the most commonly implicated pathogens is Streptococcus pneumoniae, a Gram-positive, encapsulated bacterium that exacerbates chronic bronchial inflammation, particularly in patients with underlying chronic obstructive pulmonary disease (COPD).
Microbiological and Pathogenic Profile of Streptococcus pneumoniae
S. pneumoniae possesses a polysaccharide capsule, enabling evasion from host immune responses. The organism produces pneumolysin, autolysin, and other virulence factors that facilitate adhesion to respiratory epithelium, cytotoxicity, and inflammatory cascade activation.
Virulence Mechanisms
- Capsular polysaccharides: Inhibit phagocytosis
- Pneumolysin: Lyses epithelial and immune cells
- Neuraminidase: Enhances mucosal colonization
- Biofilm formation: Promotes persistence in chronic airways
Risk Factors for Chronic Bronchitis Due to S. pneumoniae
Patients with the following risk factors are more susceptible to chronic bronchial colonization and infection by S. pneumoniae:
- Long-standing COPD or asthma
- Cigarette smoking or environmental pollutants
- Frequent respiratory tract infections
- Immunodeficiency or diabetes mellitus
- Advanced age (>65 years)
- Incomplete pneumococcal vaccination history
Clinical Manifestations of Streptococcus pneumoniae Chronic Bronchitis
Persistent Symptoms
- Chronic productive cough with purulent sputum
- Dyspnea on exertion and at rest during exacerbations
- Low-grade fever or malaise during active infection
- Wheezing and chest tightness
- Fatigue, especially in older adults
Exacerbation Triggers
- Seasonal changes
- Secondary viral infections (e.g., influenza)
- Exposure to pollutants or allergens
Diagnostic Evaluation and Confirmatory Testing
Clinical Criteria
Diagnosis of chronic bronchitis is based on symptom persistence. Pneumococcal involvement is confirmed through microbiological evidence.
Laboratory Investigations
- Sputum Gram stain and culture: Gram-positive lancet-shaped diplococci
- Polymerase Chain Reaction (PCR): For capsular gene detection
- Procalcitonin: Elevated in bacterial vs viral infections
- Complete Blood Count (CBC): Neutrophilia in active infection
- C-reactive protein (CRP) and ESR: Elevated in inflammation
Imaging
- Chest X-ray: Peribronchial thickening without lobar consolidation
- High-resolution CT (HRCT): Airway wall thickening and mucus plugging
Differential Diagnosis of Pneumococcal Chronic Bronchitis
To ensure accurate treatment, differentiation is required from:
- Viral chronic bronchitis
- Tuberculosis (especially in endemic regions)
- Bronchiectasis
- Fungal respiratory infections
- Cystic fibrosis (in younger adults)
Treatment of Chronic Bronchitis Caused by S. pneumoniae
Antibacterial Therapy
Empirical antibiotics should cover pneumococci, particularly in patients with moderate to severe symptoms or prior exacerbations.
First-Line Options
- Amoxicillin/clavulanate (preferred for outpatient treatment)
- Levofloxacin or moxifloxacin (for resistant strains or penicillin allergy)
- Cefuroxime or cefpodoxime (cephalosporins with good lung penetration)
Treatment Duration
- Typically 7 to 14 days, extended in recurrent or complicated cases
Adjunctive Therapy
- Bronchodilators (inhaled beta-agonists or anticholinergics)
- Inhaled corticosteroids for airway inflammation
- Expectorants to assist in mucus clearance
- Oxygen therapy in patients with hypoxemia
Prevention of Recurrence and Exacerbations
Immunization Strategies
- PCV13 and PPSV23 pneumococcal vaccines reduce incidence of infection and severity
- Annual influenza vaccination to prevent secondary bacterial infections
Lifestyle Modifications
- Smoking cessation
- Pulmonary rehabilitation programs
- Avoidance of occupational/environmental irritants
- Nutritional support for immunocompromised patients
Complications and Long-Term Outcomes
Potential Complications
- Frequent acute exacerbations of chronic bronchitis (AECB)
- Bronchiectasis due to repeated infection and tissue damage
- Chronic hypoxia leading to cor pulmonale
- Systemic pneumococcal spread in immunosuppressed individuals
Prognosis
Patients with early diagnosis and proper treatment typically experience controlled symptoms and improved quality of life. Prognosis worsens with poor adherence to treatment, vaccine avoidance, and persistent smoking.
Special Considerations in High-Risk Groups
Elderly and COPD Patients
- Higher susceptibility to pneumococcal colonization
- Reduced mucociliary clearance and immune responsiveness
- Often require long-term maintenance bronchodilator therapy
Immunocompromised Individuals
- May not exhibit classic symptoms
- Require broader-spectrum antibiotics initially
- Prophylactic vaccination is essential
Chronic bronchitis due to Streptococcus pneumoniae remains a significant clinical concern, especially among individuals with underlying pulmonary disease and immunosuppression. Timely diagnosis, appropriate antibiotic therapy, and preventive strategies including vaccination and lifestyle adjustments are paramount in managing disease progression and preventing recurrent exacerbations.

