Streptococcus pneumoniae bronchitis is a lower respiratory tract infection caused by Streptococcus pneumoniae, a Gram-positive, alpha-hemolytic diplococcus. Though commonly associated with pneumonia and meningitis, this pathogen is also capable of inducing bronchial inflammation, particularly in vulnerable populations such as the elderly, immunocompromised individuals, and those with chronic pulmonary disease. The clinical course ranges from mild bronchial irritation to severe, persistent bronchitis with systemic features.
Microbiological Profile of Streptococcus pneumoniae
S. pneumoniae colonizes the nasopharynx and can descend into the bronchi, especially when local defense mechanisms are impaired. It possesses several virulence factors that contribute to bronchial epithelial invasion and inflammation:
- Polysaccharide capsule: Evades phagocytosis
- Pneumolysin: Destroys epithelial cells and suppresses immune response
- Autolysin: Facilitates lysis and inflammation
- Neuraminidase: Aids in mucosal adhesion
Risk Factors and Predisposing Conditions
Several host-related and environmental factors facilitate bronchial infection by S. pneumoniae:
- Chronic obstructive pulmonary disease (COPD)
- Smoking
- Advanced age (>65 years)
- Asthma
- Immunosuppression (e.g., HIV, chemotherapy)
- Recent influenza or viral respiratory infections
- Alcohol use disorder and malnutrition
Clinical Manifestations
Common Symptoms
Patients with S. pneumoniae bronchitis typically present with:
- Persistent cough, initially dry but becoming productive
- Purulent sputum with yellow or green coloration
- Low-grade fever or chills
- Pleuritic chest pain
- Wheezing and shortness of breath
- Fatigue and malaise
Physical Examination Findings
- Rhonchi or coarse crackles on auscultation
- Wheezing or prolonged expiratory phase
- Mild hypoxemia in severe cases
Differential Diagnosis
Streptococcus pneumoniae bronchitis must be distinguished from:
- Viral bronchitis (e.g., influenza, RSV)
- Mycoplasma pneumoniae or Chlamydia pneumoniae infections
- Bacterial pneumonia
- Bronchiectasis or COPD exacerbation
- Tuberculosis (in endemic areas)
Diagnostic Evaluation
Laboratory Investigations
- Complete blood count (CBC): Leukocytosis with neutrophilia
- CRP and ESR: Elevated in bacterial infections
- Sputum Gram stain: Reveals Gram-positive diplococci
- Sputum culture: Confirms S. pneumoniae
- Procalcitonin levels: May help distinguish bacterial from viral bronchitis
Imaging
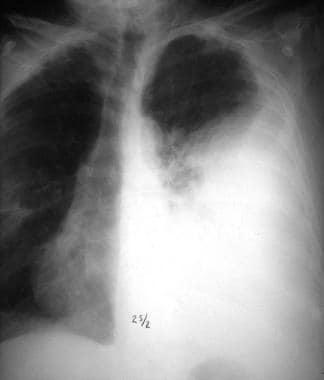
- Chest X-ray: Usually normal or shows mild peribronchial thickening
- High-resolution CT: Used in recurrent or unclear cases to rule out bronchiectasis or infiltrates
Treatment of Streptococcus pneumoniae Bronchitis
Empirical Antibiotic Therapy
Initial therapy is empirical, tailored once culture and sensitivity results are available. Effective oral antibiotics include:
- Amoxicillin-clavulanate
- Cefuroxime or cefpodoxime
- Levofloxacin or moxifloxacin (in penicillin-allergic patients)
- Azithromycin or clarithromycin (with rising resistance concerns)
Duration
- Treatment typically lasts 7 to 10 days, depending on clinical response and comorbidities.
Supportive Measures
- Hydration and humidified air to soothe bronchial mucosa
- Bronchodilators: In patients with wheezing or underlying asthma/COPD
- Antipyretics and analgesics: For fever and discomfort
- Avoidance of cough suppressants: To promote sputum clearance
Preventive Strategies
Vaccination
- Pneumococcal conjugate vaccine (PCV13)
- Pneumococcal polysaccharide vaccine (PPSV23) for high-risk adults
- Annual influenza vaccination to reduce secondary bacterial infections
Risk Factor Mitigation
- Smoking cessation
- Management of chronic lung diseases
- Minimizing exposure to respiratory pathogens in healthcare settings
Complications and Chronic Outcomes
Untreated or recurrent S. pneumoniae bronchitis can lead to:
- Secondary bacterial pneumonia
- Chronic bronchitis or COPD exacerbations
- Bronchiectasis in recurrent cases
- Sepsis in immunocompromised individuals
Special Considerations in Vulnerable Populations
Elderly Patients
- May exhibit atypical symptoms such as confusion or lethargy
- More likely to develop complications and require hospitalization
Immunocompromised Individuals
- Require broader antibiotic coverage initially
- Prophylactic vaccination is imperative
Prognosis
When promptly treated, streptococcus pneumoniae bronchitis has an excellent prognosis. Most immunocompetent individuals recover fully without sequelae. The outcome worsens in elderly or chronically ill patients if diagnosis is delayed or antibiotic resistance is encountered.
Streptococcus pneumoniae bronchitis remains an under-recognized but clinically significant lower respiratory tract infection. Prompt clinical recognition, accurate microbiological diagnosis, and early antibiotic administration are essential for optimal outcomes. Preventive strategies including vaccination and chronic disease management play a critical role in reducing incidence and morbidity.