Streptococcus pericarditis is an acute or subacute inflammation of the pericardial sac, caused by various Streptococcus species. Though rare in the antibiotic era, this form of bacterial pericarditis remains a critical and life-threatening condition if not promptly diagnosed and managed. The infection typically results in purulent pericardial effusion, rapid clinical deterioration, and potential progression to cardiac tamponade or constrictive pericarditis.
Etiology and Pathogenic Mechanisms
The primary streptococcal pathogens implicated in pericarditis include:
- Streptococcus pneumoniae: Most common in pneumococcal infections spreading hematogenously or via contiguous lung infection.
- Streptococcus pyogenes (GAS): Associated with severe soft tissue infections and sepsis.
- Streptococcus agalactiae (GBS): Increasingly identified in immunocompromised adults.
- Viridans group streptococci: Often linked to endocarditis with pericardial involvement.
Risk Factors and Predisposing Conditions
Several factors increase susceptibility to streptococcal pericarditis:
- Recent pneumonia or pleural empyema
- Cardiac or thoracic surgery
- Immunosuppression or neutropenia
- Hematologic malignancies
- Diabetes mellitus
- Pericardial injury or post-traumatic states
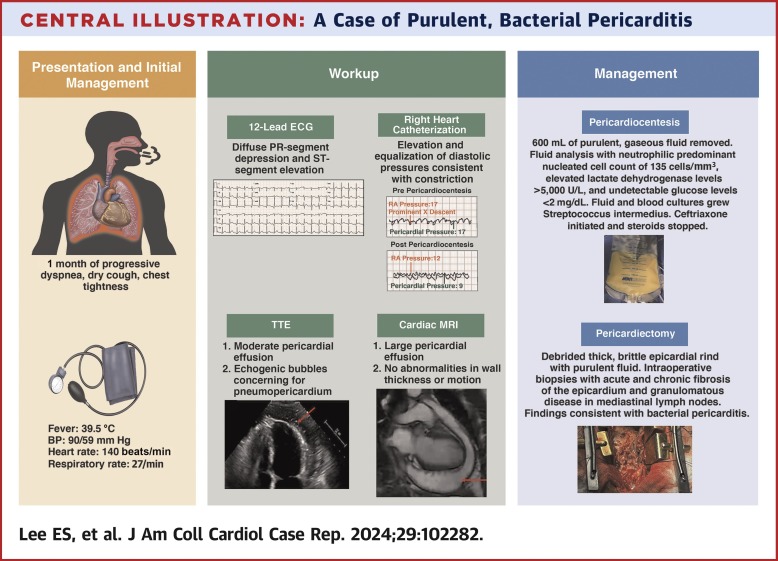
Clinical Features of Streptococcus-Induced Pericarditis
Symptoms
- Chest pain: Sharp and pleuritic, often relieved by sitting forward
- Fever and chills: Hallmarks of bacterial infection
- Dyspnea and orthopnea: Due to pericardial effusion
- Tachycardia and hypotension
- Muffled heart sounds and jugular venous distention (JVD)
Signs of Tamponade
- Pulsus paradoxus
- Low voltage QRS complexes on ECG
- Electrical alternans
- Beck’s triad: Hypotension, JVD, and muffled heart sounds
Diagnostic Workup
Laboratory Investigations
- CBC: Leukocytosis with left shift
- CRP/ESR: Elevated inflammatory markers
- Blood cultures: Crucial for identifying Streptococcus spp.
- Pericardial fluid analysis: Gram stain, culture, and cytology
Imaging Studies
- Echocardiography: First-line for detecting pericardial effusion and tamponade
- Chest X-ray: May show enlarged cardiac silhouette
- ECG: Diffuse ST-segment elevation, PR depression
- CT/MRI: Advanced imaging for constriction or effusion characterization
Pericardial Fluid Characteristics
| Feature | Streptococcus Pericarditis |
|---|---|
| Appearance | Purulent, cloudy |
| WBC count | >100,000/mm³ |
| Protein | Elevated |
| LDH | High |
| Glucose | Markedly decreased |
| Gram stain | Positive for Streptococcus |
| Culture | Usually positive |
Management and Treatment Protocols
Medical Management
Empirical intravenous antibiotics must be initiated immediately upon suspicion of bacterial pericarditis, especially with signs of systemic toxicity or tamponade.
- Empiric therapy:
- Vancomycin: Coverage for resistant strains
- Ceftriaxone or Cefotaxime: Effective against S. pneumoniae and GAS
- Adjust antibiotics based on culture sensitivity
Duration
- Minimum 4 weeks of antibiotic therapy, typically initiated intravenously
Adjunctive Measures
- NSAIDs or corticosteroids: For inflammation (only after ruling out active infection)
- Colchicine: Limited role; mainly in recurrent pericarditis
Surgical and Interventional Strategies
Indications for Pericardial Drainage
- Hemodynamic instability
- Large or loculated effusions
- Purulent or hemorrhagic fluid
- Failed medical management
Surgical Options
- Pericardiocentesis: Initial intervention for tamponade
- Pericardial window: For ongoing drainage
- Pericardiectomy: In constrictive pericarditis cases
Complications of Streptococcus Pericarditis
If left untreated or inadequately managed, complications include:
- Cardiac tamponade
- Constrictive pericarditis
- Myopericarditis
- Septicemia and metastatic infections
- Death (mortality rates remain high without prompt intervention)
Prognosis and Outcomes
With early identification and aggressive treatment, the prognosis improves significantly. However, delays in diagnosis may result in irreversible cardiac compromise. Mortality rates in untreated purulent pericarditis can exceed 40%.
Prevention and Prophylaxis
- Prompt treatment of respiratory streptococcal infections
- Pneumococcal vaccination, especially in high-risk groups
- Strict asepsis during cardiac procedures
- Monitoring and prophylaxis in immunocompromised patients
Streptococcus pericarditis is a rare yet emergent infectious pathology of the pericardium. Given its aggressive course and high mortality, especially in purulent presentations, clinicians must maintain a high index of suspicion in relevant clinical settings. Rapid initiation of antibiotic therapy, timely drainage procedures, and close monitoring are essential to achieving favorable outcomes. Preventive strategies in at-risk populations remain crucial in minimizing incidence and complications.

