Streptococcus myositis is a rare but fulminant infection of skeletal muscle primarily caused by Group A Streptococcus (GAS), most notably Streptococcus pyogenes. It is distinct from pyomyositis due to the absence of abscess formation and its rapid necrotizing nature. If left untreated, the condition can quickly lead to systemic toxicity, multi-organ failure, and death.
This aggressive form of necrotizing myositis requires early recognition and immediate intervention to avoid fatal outcomes. The infection is predominantly monomicrobial, with GAS as the principal etiologic agent, known for its ability to produce potent exotoxins and enzymes that destroy tissue and evade the host immune system.

Etiological Agent: Group A Streptococcus in Muscle Infections
Pathogenic Features of Streptococcus pyogenes
- M protein: Inhibits phagocytosis and promotes adhesion.
- Streptolysins O and S: Cause direct muscle cell lysis.
- Exotoxins (SPEs): Act as superantigens triggering cytokine storm.
- Hyaluronidase and streptokinase: Facilitate tissue invasion and spread.
The combination of these virulence factors explains the rapid tissue destruction, systemic inflammatory response, and high mortality rate associated with streptococcal myositis.
Risk Factors for Streptococcal Myositis
While the infection can occur in previously healthy individuals, several risk factors are associated with increased susceptibility:
- Recent trauma or muscle strain (even minor)
- Intramuscular injections
- Varicella zoster virus infection
- Diabetes mellitus
- Immunocompromised status
- NSAID use masking early symptoms
Clinical Presentation: Signs and Symptoms of Streptococcus Myositis
Early Stage:
- Severe, disproportionate pain localized to a muscle group
- Rapid onset of swelling and erythema
- Tenderness with minimal overlying skin changes
- Fever, malaise, and chills
Progressive Stage:
- Rapid progression to compartment syndrome
- Cutaneous signs: edema, bullae, skin discoloration
- Crepitus and subcutaneous gas are uncommon (differentiates from gas gangrene)
- Systemic toxicity: hypotension, tachycardia, altered mental status
- Septic shock and multi-organ failure
Diagnostic Approach to Streptococcus Myositis
Laboratory Tests:
- Leukocytosis with left shift
- Elevated creatine kinase (CK) and myoglobin
- Elevated C-reactive protein (CRP) and ESR
- Blood cultures: Often positive for S. pyogenes
- Lactic acidosis may indicate systemic compromise
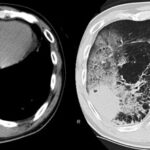
Imaging:
- MRI with contrast: Gold standard for identifying muscle inflammation and necrosis
- CT scan: May reveal muscle edema but lacks soft tissue specificity
- Ultrasound: Limited utility in deep muscle infections
Surgical Exploration:
In most cases, definitive diagnosis is achieved via early surgical debridement, allowing for culture, histopathology, and confirmation of myonecrosis.
Differential Diagnosis of Muscle Infections
- Necrotizing fasciitis: Primarily involves fascia; may coexist with myositis
- Clostridial myonecrosis (gas gangrene): Caused by Clostridium perfringens; gas production common
- Pyomyositis: Typically staphylococcal; abscess formation present
- Inflammatory myopathies: Chronic course and autoimmune markers
- Deep vein thrombosis: Mimics pain and swelling but lacks systemic toxicity
Treatment of Streptococcus Myositis
Immediate Management:
- Initiate empirical broad-spectrum IV antibiotics:
- Penicillin G + Clindamycin (clindamycin inhibits toxin production)
- Add vancomycin or linezolid if MRSA cannot be ruled out
- Early aggressive surgical debridement:
- Removal of all necrotic tissue is critical to halting disease progression
- Often requires multiple surgeries
Supportive Measures:
- Intensive care for hemodynamic stabilization
- Fluid resuscitation and vasopressors as needed
- Monitoring for renal failure due to rhabdomyolysis
- Mechanical ventilation if respiratory muscles are involved
Adjunctive Therapy:
- Intravenous immunoglobulin (IVIG) may help neutralize streptococcal exotoxins in toxic shock
- Hyperbaric oxygen therapy: Limited evidence but may be beneficial in selected cases
Complications of Untreated or Late-Diagnosed Streptococcus Myositis
- Septicemia with high mortality
- Acute renal failure due to rhabdomyolysis
- Limb amputation due to irreversible necrosis
- Disseminated intravascular coagulation (DIC)
- Multi-organ failure
- Residual myopathy or functional disability
Prompt surgical and antimicrobial therapy remains the only reliable means of reducing morbidity and mortality.
Prognosis and Outcomes
Streptococcus myositis has a high case fatality rate, often exceeding 30–40% when diagnosis and intervention are delayed. Outcomes are significantly improved with:
- Rapid recognition and diagnosis
- Early surgical intervention (within 12–24 hours)
- Aggressive supportive care
- Source control and appropriate antibiotics
Preventive Strategies
General Measures:
- Proper wound hygiene and early treatment of superficial skin infections
- Caution with intramuscular injections, especially in high-risk patients
- Early evaluation of unexplained muscle pain or systemic symptoms
Specific Populations:
- Varicella patients: Monitor closely for signs of soft tissue infection
- Avoid NSAIDs in suspected streptococcal infections due to potential masking of symptoms and worsened outcomes
Streptococcus myositis represents a medical emergency demanding high clinical suspicion, rapid diagnosis, and immediate multidisciplinary intervention. Group A Streptococcus pyogenes acts as the primary agent, utilizing potent exotoxins and invasive mechanisms to cause widespread muscle necrosis and systemic collapse. Early surgical debridement combined with targeted antibiotics and intensive care support is essential for survival. With increasing recognition and prompt action, outcomes can significantly improve, but delays remain deadly.