Streptococcus empyema refers to the accumulation of pus in the pleural space due to infection by streptococcal bacteria, most commonly Streptococcus pneumoniae, though Streptococcus anginosus group and Group A Streptococcus may also be implicated. This condition represents a severe form of parapneumonic effusion and is often associated with significant morbidity, especially in children and immunocompromised individuals.
Pathogenesis of Streptococcus-Induced Pleural Empyema
Streptococcal empyema typically develops as a complication of pneumonia. The infection progresses through three pathological stages:
- Exudative Stage: Sterile fluid accumulates in the pleural space.
- Fibrinopurulent Stage: Bacterial invasion, fibrin deposition, and neutrophilic infiltration occur.
- Organizing Stage: Fibroblast proliferation leads to thickened pleura and potential lung entrapment.
Streptococcal species utilize various virulence factors including pneumolysin, streptolysin O, and capsule polysaccharides to evade immune clearance and promote rapid pleural involvement.
Common Streptococcal Pathogens in Empyema
1. Streptococcus pneumoniae
The leading cause of community-acquired empyema in both pediatric and adult populations, especially post-pneumococcal infections.
2. Streptococcus anginosus group (SAG)
Includes S. anginosus, S. intermedius, and S. constellatus; known for abscess formation and often involved in polymicrobial pleural infections.
3. Group A Streptococcus (S. pyogenes)
Though rare, it can cause rapidly progressive empyema and necrotizing pleural infections, especially in post-viral respiratory infections.
Clinical Features of Streptococcus Empyema
Symptoms:
- Pleuritic chest pain
- Dyspnea and tachypnea
- Persistent high-grade fever
- Productive cough with purulent sputum
- Decreased breath sounds and dullness to percussion
Signs in Severe Cases:
- Sepsis or septic shock
- Weight loss, malaise, night sweats
- Hypoxemia and respiratory distress
Children may exhibit irritability, poor feeding, and abdominal pain.
Diagnostic Approach to Streptococcal Empyema
Imaging:
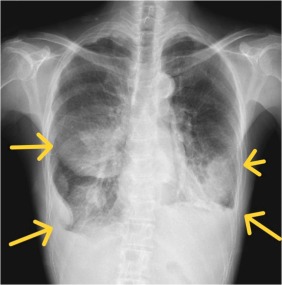
- Chest X-ray: Blunting of costophrenic angle, pleural opacity
- Ultrasound: Identifies septations, loculated fluid, and guides drainage
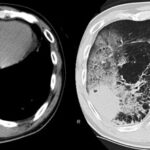
- CT Thorax: Detailed assessment of pleural space, lung entrapment, and abscesses
Laboratory Evaluation:
- Thoracentesis with Pleural Fluid Analysis
- Appearance: Purulent, turbid
- pH < 7.2
- Glucose < 40 mg/dL
- LDH > 1000 IU/L
- Positive Gram stain/culture for Streptococcus spp.
- Blood Cultures: Often positive in S. pneumoniae infections
- PCR assays: Detect pneumococcal DNA when cultures are negative
Antimicrobial Therapy for Streptococcus Empyema
Prompt, broad-spectrum empirical antibiotic therapy is initiated and refined based on culture and sensitivity results.
Empirical Therapy:
- Ceftriaxone or cefotaxime + vancomycin (for S. pneumoniae, including resistant strains)
- Ampicillin-sulbactam or piperacillin-tazobactam (effective against SAG)
- Clindamycin: Added for toxin inhibition in S. pyogenes or mixed anaerobic infections
Targeted Therapy (Duration: 2–4 weeks):
- S. pneumoniae: High-dose penicillin or ceftriaxone
- SAG: Ampicillin or amoxicillin-clavulanate
- GAS: Penicillin + clindamycin
Pleural Drainage and Surgical Management
Effective drainage is critical to resolving empyema and preventing chronic pleural fibrosis.
Drainage Options:
- Intercostal chest tube drainage: For free-flowing or mildly loculated collections
- Intrapleural fibrinolytics (e.g., alteplase + DNase): Improve drainage in multiloculated empyemas
- Video-Assisted Thoracoscopic Surgery (VATS): Indicated when drainage fails or in organizing stage
- Open decortication: Reserved for chronic empyema with trapped lung
Timely intervention reduces hospital stay, need for reoperation, and long-term lung dysfunction.
Prognosis and Complications
Streptococcal empyema, when promptly managed, has a favorable prognosis. However, complications may arise:
- Pleural thickening
- Bronchopleural fistula
- Persistent sepsis or bacteremia
- Lung entrapment and restrictive ventilatory defect
- Mortality (higher in elderly and delayed treatment)
Prevention Strategies and Vaccination
Pneumococcal Vaccination:
- PCV13 and PPSV23 have significantly reduced invasive pneumococcal diseases, including empyema.
- Recommended for children, adults >65, and immunocompromised individuals.
Early Management of Pneumonia:
- Reduces risk of parapneumonic complications
- Close monitoring of high-risk patients helps identify progression to empyema early
Streptococcus empyema represents a serious progression of pulmonary infection requiring prompt recognition, targeted antibiotic therapy, and effective pleural drainage. Streptococcus pneumoniae remains the predominant cause, with rising concerns about antimicrobial resistance. A multidisciplinary approach involving infectious disease, radiology, and thoracic surgery optimizes outcomes and prevents chronic complications. Prevention through pneumococcal vaccination remains a cornerstone in reducing the burden of streptococcal empyema worldwide.