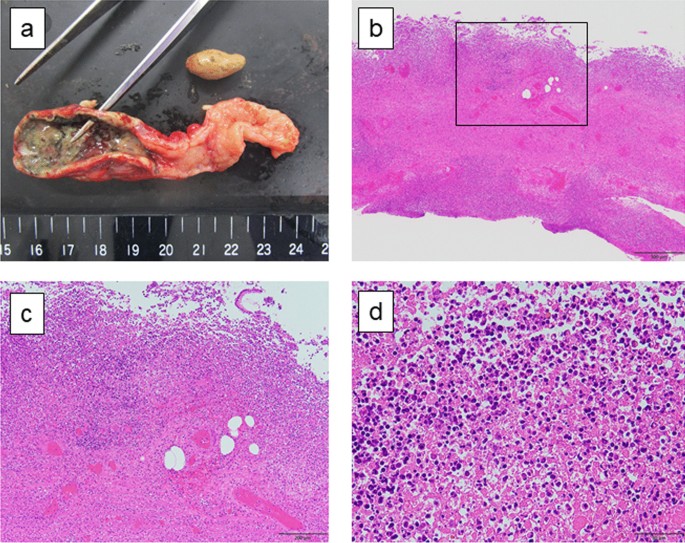
Complicated appendicitis—characterized by perforation, gangrene, or abscess formation—is an acute, life-threatening condition that often results from microbial invasion of the appendix. Among the bacterial pathogens implicated, Streptococcus pyogenes (Group A Streptococcus), and less commonly Streptococcus anginosus group, play a critical role in exacerbating inflammation and promoting rapid progression to sepsis and peritonitis.
Pathophysiological Role of Streptococcus in Appendiceal Inflammation
Streptococcal species contribute to severe appendiceal infection through their virulence factors, such as exotoxins, M proteins, and streptolysins. These components breach host barriers, disrupt immune responses, and accelerate necrosis and tissue destruction, thereby transitioning a simple appendicitis to a complicated form.
The process is frequently polymicrobial but often dominated by streptococci in culture-positive cases of perforated or gangrenous appendicitis.
Clinical Presentation of Streptococcus-Associated Complicated Appendicitis
Typical Symptoms:
- Severe right lower quadrant abdominal pain
- Fever (>38.5°C)
- Nausea, vomiting, and anorexia
- Diffuse abdominal tenderness or guarding (if peritonitis develops)
Systemic Signs Suggestive of Streptococcal Sepsis:
- Hypotension
- Tachycardia
- Elevated serum lactate
- Signs of multi-organ dysfunction (in advanced cases)
Children and immunocompromised patients are particularly vulnerable to fulminant progression.
Microbiological Insights and Common Isolates
Studies have shown that Streptococcus pyogenes, Streptococcus anginosus, and other β-hemolytic streptococci are isolated more frequently in complicated appendicitis cases than in uncomplicated ones. These organisms often coexist with anaerobes such as Bacteroides fragilis, creating a synergistic infection profile.
Common Streptococcal Isolates:
- Streptococcus pyogenes (GAS) – associated with necrotizing inflammation
- Streptococcus anginosus group – linked to abscess formation
- Streptococcus constellatus – prominent in intra-abdominal infections
Diagnostic Strategies for Complicated Appendicitis with Streptococcus
Imaging:
- Contrast-enhanced CT scan is the modality of choice for evaluating appendiceal rupture, abscess, and peritonitis.
- Ultrasound is preferred in children and pregnant women, though less sensitive in detecting perforation.
Laboratory Indicators:
- Elevated white blood cell count with a left shift
- High C-reactive protein (CRP) and procalcitonin
- Blood cultures: Essential for identifying systemic Streptococcal bacteremia
- Peritoneal fluid culture (if surgical drainage performed): Identifies specific streptococcal strains
Antibiotic Management of Streptococcus-Complicated Appendicitis
Immediate empirical antimicrobial therapy is crucial to managing streptococcal involvement and preventing septic complications.
Empirical Therapy:
- Piperacillin-tazobactam or ceftriaxone + metronidazole: Covers Gram-positive cocci, Gram-negatives, and anaerobes
- Vancomycin: Considered in patients at risk for methicillin-resistant streptococcal strains or those with toxic shock signs
Pathogen-Specific Therapy (upon culture results):
- Penicillin G + clindamycin: Preferred regimen for Streptococcus pyogenes, clindamycin reduces toxin production
- Ampicillin-sulbactam: Effective for Streptococcus anginosus group infections
Duration:
- 7–10 days for most cases
- Extended if abscess or sepsis is present or surgical drainage was incomplete
Surgical Management and Postoperative Care
Appendectomy:
- Laparoscopic appendectomy is standard and offers lower postoperative morbidity.
- Open appendectomy may be required in cases of diffuse peritonitis or large abscesses.
Drainage:
- Percutaneous abscess drainage guided by CT or ultrasound is essential for abscess control and is often combined with antibiotics.
Postoperative Monitoring:
- Monitor for signs of ongoing infection: fever, leukocytosis, or persistent pain
- Repeat imaging if clinical status deteriorates
- Consider infectious disease consultation for recurrent or invasive streptococcal infections
Complications and Mortality
Complicated appendicitis involving Streptococcus pyogenes or S. anginosus can lead to severe, often fatal complications if not promptly managed:
- Generalized peritonitis
- Septic shock
- Necrotizing fasciitis (rare but aggressive)
- Intra-abdominal abscess
- Wound infection and dehiscence
- Multisystem organ failure
Early diagnosis, aggressive antimicrobial therapy, and timely surgical intervention significantly reduce mortality.
Preventive Considerations and Prognostic Outlook
While there is no vaccine currently approved for prevention of appendicitis, broader hygiene practices and awareness of early symptoms may reduce progression to complicated stages.
Patients recovering from streptococcal appendicitis require:
- Completion of full antibiotic course
- Postoperative wound care
- Long-term follow-up if abscess or severe infection occurred
Prognosis is favorable with early, aggressive management, but delay in treatment correlates with increased morbidity and extended hospitalization.
Streptococcus species are important, often underrecognized contributors to complicated appendicitis. Their aggressive virulence factors make them key culprits in perforation, abscess formation, and peritonitis. Accurate recognition, prompt imaging, targeted antibiotics, and timely surgical intervention form the foundation of successful outcomes. A high index of suspicion for streptococcal involvement is essential in cases exhibiting severe systemic symptoms or rapid clinical deterioration.

