Streptococcal septicemia, also referred to as streptococcal bacteremia, is a critical bloodstream infection caused by invasive strains of Streptococcus species. This condition demands urgent clinical attention due to its high risk of systemic complications such as septic shock, multi-organ failure, and death. The most common causative organisms are Group A Streptococcus (GAS) and Group B Streptococcus (GBS), though other species including Streptococcus pneumoniae and Streptococcus anginosus may also be implicated.

Pathophysiology of Streptococcal Septicemia
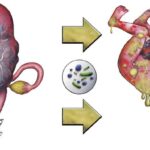
Streptococcal septicemia develops when pathogenic streptococci gain access to the bloodstream, either through direct invasion from a local infection site or secondary to mucosal barrier disruption. The bacteria rapidly multiply and release exotoxins and superantigens, which lead to systemic inflammatory responses and vascular dysfunction.
Etiologic Agents and Their Clinical Profiles
Group A Streptococcus (Streptococcus pyogenes)
- Highly virulent, beta-hemolytic
- Causes pharyngitis, cellulitis, necrotizing fasciitis, and toxic shock syndrome
- Rapid progression to septicemia, particularly in skin and soft tissue infections
Group B Streptococcus (Streptococcus agalactiae)
- Commonly affects neonates, pregnant women, and elderly individuals
- Associated with urinary tract infections, pneumonia, and meningitis
- Can result in early-onset or late-onset neonatal sepsis
Other Streptococcal Species
- Streptococcus pneumoniae: Often leads to bacteremic pneumonia or meningitis
- Streptococcus anginosus group: Associated with abscess formation and deep tissue infections
- Viridans streptococci: Frequently implicated in endocarditis, especially in immunocompromised hosts
Epidemiology and Risk Factors
Streptococcal septicemia can occur in any age group but is most prevalent among:
- Neonates (GBS vertical transmission)
- Elderly adults
- Individuals with diabetes, cancer, HIV/AIDS
- Patients with indwelling medical devices
- Post-surgical or trauma patients
- Immunosuppressive therapy recipients
The seasonal peak of GAS-related infections occurs in winter and early spring.
Clinical Manifestations of Streptococcal Septicemia
Streptococcal septicemia often presents with rapid-onset systemic symptoms that escalate quickly if untreated:
- High-grade fever and rigors
- Hypotension and tachycardia
- Altered mental status
- Signs of localized infection (e.g., cellulitis, pharyngitis, wound infection)
- Respiratory distress or hypoxia
- Petechiae or purpura (in toxic streptococcal syndrome)
- Multi-organ dysfunction in advanced stages
The clinical course may deteriorate swiftly, necessitating intensive care.
Diagnostic Evaluation
Clinical Workup
- Thorough history: Recent infections, wounds, surgeries, or systemic symptoms
- Physical examination: Assess for signs of local and systemic infection
Laboratory Investigations
- Blood cultures (before antibiotics): Identify streptococcal species
- CBC: Leukocytosis or leukopenia
- CRP and Procalcitonin: Elevated in systemic infection
- Lactate levels: Marker for sepsis-induced hypoperfusion
- Renal and hepatic function panels: Monitor for organ failure
- Coagulation profile: Identify DIC if suspected
Imaging
- Chest X-ray or CT scan: Rule out pneumonia or abscesses
- Echocardiography: Evaluate for endocarditis in suspected cases
Treatment and Management of Streptococcal Septicemia
Immediate Resuscitation
- Airway and oxygenation: Supplemental oxygen or intubation if necessary
- Fluid resuscitation: 30 mL/kg crystalloids within the first hour
- Vasopressors: Initiate if hypotension persists after fluids
- Continuous monitoring in ICU for severe cases
Empirical Antimicrobial Therapy
Treatment must begin immediately upon suspicion, even before culture confirmation:
- Penicillin G + Clindamycin: Gold standard for invasive GAS infections
- Ampicillin + Gentamicin: Preferred for GBS septicemia
- Vancomycin: If resistance or MRSA co-infection is a concern
- Modify antibiotics based on sensitivity profiles once available
Clindamycin is crucial in toxin suppression for GAS infections.
Supportive Care
- Renal replacement therapy: For acute kidney injury
- Mechanical ventilation: In respiratory failure
- Blood transfusions and coagulation support: If DIC occurs
- Nutritional and electrolyte support: For critically ill patients
Complications and Prognostic Indicators
If not promptly managed, streptococcal septicemia can result in:
- Septic shock
- Acute respiratory distress syndrome (ARDS)
- Disseminated intravascular coagulation (DIC)
- Endocarditis
- Abscess formation
- Neonatal cerebral palsy or death (in GBS)
Prognosis depends on the time to antibiotic administration, host immune status, and early critical care intervention. Mortality rates range from 15% to 45% in severe cases.
Prevention Strategies
Neonatal and Maternal Health
- Universal GBS screening in pregnant women (35–37 weeks)
- Intrapartum antibiotic prophylaxis in GBS-positive mothers
- Sterile delivery practices and neonatal monitoring
General Public Health Measures
- Prompt treatment of streptococcal pharyngitis and skin infections
- Strict aseptic techniques in hospitals and clinics
- Vigilant wound care and hygiene education
- Vaccination for S. pneumoniae in vulnerable populations
Antimicrobial Stewardship
- Rational use of antibiotics to prevent resistance
- Surveillance of invasive streptococcal strains in community and hospital settings
Streptococcal septicemia is an aggressive bloodstream infection with the potential for catastrophic systemic outcomes. Through prompt recognition, immediate initiation of broad-spectrum antibiotics, and supportive critical care, the disease course can be significantly altered in favor of patient survival. Clinicians must maintain a high index of suspicion in at-risk populations and implement effective infection control and prevention protocols to minimize the impact of this life-threatening condition.