Streptococcal septic abortion is a severe, often life-threatening infection of the uterine cavity occurring after an abortion, induced or spontaneous. This condition is commonly caused by Group A Streptococcus (Streptococcus pyogenes) and Group B Streptococcus (Streptococcus agalactiae), which can lead to rapid-onset sepsis, endometritis, and multisystem organ failure if not identified and treated promptly. Recognizing this emergency early is critical in reducing maternal morbidity and mortality.
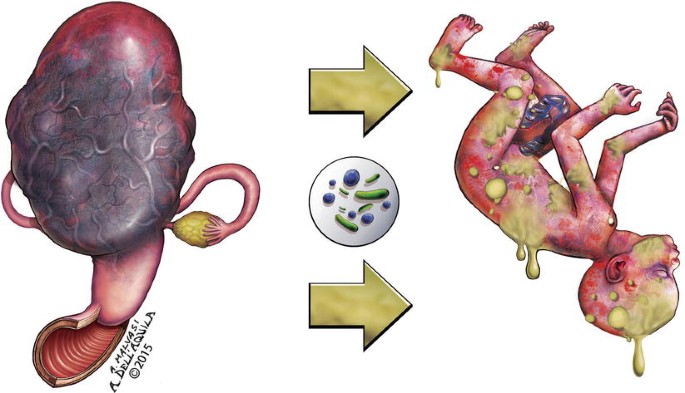
Pathogenesis of Streptococcal Septic Abortion
The pathogenesis typically begins with the ascension of pathogenic streptococcal bacteria into the uterine cavity following abortion. Tissue disruption, retained products of conception, or non-sterile procedures promote bacterial proliferation. Invasive streptococcal species produce exotoxins and superantigens that trigger massive systemic inflammatory responses, progressing rapidly to septic shock.
Epidemiology and Risk Factors
Although relatively rare in regions with access to sterile medical care, streptococcal septic abortion still occurs and poses high risk in certain populations and contexts:
- Unsafe or illegal abortions
- Incomplete abortions with retained products
- Non-sterile surgical instruments or practices
- Pre-existing vaginal or systemic streptococcal colonization
- Immunocompromised patients (HIV, diabetes)
- Delayed post-abortion care
Women in low-resource or restrictive healthcare environments are particularly vulnerable.
Clinical Presentation and Symptoms
Symptoms of streptococcal septic abortion often manifest acutely within hours to days following an abortion procedure or spontaneous miscarriage. Hallmark signs include:
- High-grade fever (>38.5°C) and chills
- Foul-smelling vaginal discharge
- Severe abdominal or pelvic pain
- Uterine tenderness
- Tachycardia and hypotension
- Confusion or altered mental status
- Signs of septic shock (cold extremities, cyanosis, oliguria)
The clinical course may deteriorate rapidly, underscoring the need for immediate evaluation and intervention.
Diagnostic Evaluation
Clinical Assessment
- Vital signs: Persistent hypotension, tachycardia, and fever
- Pelvic examination: Uterine tenderness, cervical motion pain, and purulent discharge
- History: Recent abortion or miscarriage, possible unregulated procedure
Laboratory Tests
- Complete blood count (CBC): Leukocytosis or leukopenia
- Blood cultures: To isolate S. pyogenes, S. agalactiae, or polymicrobial flora
- Endometrial cultures: Confirm intrauterine infection
- CRP and Procalcitonin: Elevated inflammatory markers
- Lactic acid: Elevated levels may indicate tissue hypoperfusion and sepsis
Imaging
- Transvaginal ultrasound: Evaluate for retained products of conception, uterine perforation, or abscess formation
Microbial Etiology: Focus on Streptococcal Species
Group A Streptococcus (Streptococcus pyogenes)
- Produces streptolysins, exotoxins, and M protein
- High risk for toxic shock syndrome
- Rapid disease progression with high mortality
Group B Streptococcus (Streptococcus agalactiae)
- Common vaginal colonizer
- Severe infections in pregnant or postpartum women
- Less fulminant than GAS but still associated with sepsis
Polymicrobial infections involving anaerobes and gram-negative rods may co-exist, particularly in unsafe abortion cases.
Differential Diagnosis
Conditions with overlapping symptoms must be ruled out:
- Pelvic inflammatory disease (PID)
- Postpartum endometritis
- Incomplete abortion without sepsis
- Ectopic pregnancy rupture
- Appendicitis
- Pyelonephritis
Timely distinction through imaging, cultures, and clinical findings is essential.
Treatment and Emergency Management
Immediate Stabilization
- Airway, Breathing, Circulation (ABCs)
- IV fluid resuscitation with isotonic crystalloids
- Vasopressors if hypotension persists after fluids
- Monitor for disseminated intravascular coagulation (DIC) or acute respiratory distress syndrome (ARDS)
Empirical Antibiotic Therapy
Initiated immediately before culture results:
- First-line regimen:
- Clindamycin + Gentamicin ± Ampicillin
- OR Piperacillin-tazobactam for broader coverage
- Consider Vancomycin if MRSA suspected
- Modify regimen based on culture sensitivity
Clindamycin is particularly effective in suppressing streptococcal toxin production.
Surgical Intervention
- Uterine evacuation: Remove retained products of conception
- Hysterectomy: May be required in cases of uterine necrosis or uncontrolled infection
- Debridement of necrotic tissue in pelvic sepsis
Complications and Prognosis
If untreated or diagnosed late, streptococcal septic abortion can progress to:
- Septic shock
- Acute kidney injury (AKI)
- Multi-organ failure
- Infertility due to uterine damage
- Death, especially in Group A Streptococcus infections
Prompt treatment significantly improves survival, with outcomes depending on time to diagnosis and therapeutic response.
Prevention and Public Health Considerations
Safe Abortion Practices
- Promote access to legal, sterile abortion services
- Adequate pre-procedure screening for streptococcal colonization
- Prophylactic antibiotics in high-risk patients
Post-Abortion Care
- Educate patients on warning signs of infection
- Encourage follow-up care within 7–14 days
- Ensure complete uterine evacuation using ultrasound if needed
Broader Interventions
- Advocate for reproductive health rights and access
- Strengthen infection control protocols in healthcare settings
- Monitor for streptococcal outbreaks in obstetric wards
Streptococcal septic abortion represents a critical medical emergency requiring rapid recognition, aggressive antibiotic therapy, and often surgical management. Early diagnosis remains the cornerstone for favorable outcomes. As healthcare providers, we must ensure that patients receive safe abortion services, education, and vigilant post-procedural monitoring to prevent avoidable complications and fatalities.