Streptococcal pneumonia, commonly referred to as pneumococcal pneumonia, is a severe bacterial infection of the lungs caused by Streptococcus pneumoniae. This gram-positive diplococcus is a leading cause of community-acquired pneumonia worldwide and is responsible for considerable morbidity and mortality, particularly in vulnerable populations such as infants, the elderly, and immunocompromised individuals.
Pathogenesis of Streptococcus pneumoniae Infection
The development of streptococcal pneumonia begins with colonization of the nasopharynx, followed by invasion into the lower respiratory tract. The organism evades host immune defenses through its polysaccharide capsule, which inhibits phagocytosis. It induces a robust inflammatory response, leading to alveolar exudate accumulation, impaired gas exchange, and clinical pneumonia.
Epidemiology and Risk Factors
Streptococcal pneumonia remains a major cause of illness globally, particularly in:
- Children under 5 and adults over 65
- Individuals with chronic illnesses (COPD, diabetes, heart disease)
- Smokers
- People with weakened immune systems (e.g., HIV infection, cancer, post-splenectomy)
- Residents of nursing homes and long-term care facilities
Seasonal peaks are noted during the winter months, coinciding with viral respiratory infections which predispose to bacterial superinfection.
Clinical Presentation of Streptococcal Pneumonia
Patients typically present with a sudden onset of symptoms, including:
- High-grade fever and chills
- Pleuritic chest pain
- Productive cough with rusty or purulent sputum
- Dyspnea and tachypnea
- Fatigue and malaise
- Crackles or rales on auscultation
- Signs of consolidation (dullness to percussion, increased vocal fremitus)
In older adults, symptoms may be atypical, with confusion, hypothermia, or falls being early indicators.
Diagnostic Criteria and Investigations
Physical Examination
- Respiratory rate >30/min, crackles, bronchial breath sounds, egophony
- Signs of respiratory distress in severe cases
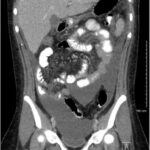
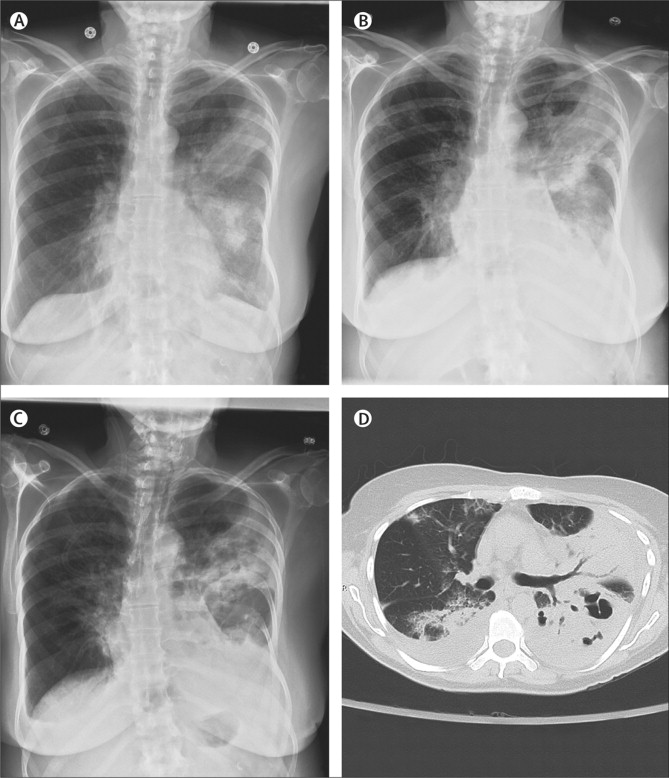
Radiological Findings
- Chest X-ray: Lobar consolidation is classic for pneumococcal pneumonia, most often in the lower lobes
Laboratory Tests
- Complete blood count (CBC): Leukocytosis with neutrophilia
- Blood cultures: Positive in ~20-30% of bacteremic cases
- Sputum Gram stain: Gram-positive, lancet-shaped diplococci
- Urinary antigen test: Detects pneumococcal C-polysaccharide antigen
- Procalcitonin and C-reactive protein (CRP): Indicators of bacterial infection
Differential Diagnosis
Streptococcal pneumonia should be differentiated from:
- Viral pneumonia (influenza, RSV)
- Atypical pneumonia (Mycoplasma, Legionella)
- Tuberculosis
- Aspiration pneumonia
- Pulmonary embolism
Correct identification is critical to ensure timely and appropriate treatment.
Treatment Protocols and Antibiotic Management
Empiric Antibiotic Therapy
Initiate based on severity and comorbidities:
- Mild cases (outpatients):
- Amoxicillin or doxycycline
- Macrolides (e.g., azithromycin) in low-resistance areas
- Moderate to severe (hospitalized patients):
- Beta-lactam (e.g., ceftriaxone or cefotaxime) + macrolide
- Alternatively, respiratory fluoroquinolone (e.g., levofloxacin)
- ICU admission or bacteremia:
- High-dose intravenous penicillin G or cefotaxime
- Add vancomycin or linezolid if MRSA or resistant strains are suspected
Duration: Generally 5–7 days; extended in complicated cases
Supportive Care
- Oxygen supplementation
- Antipyretics and analgesics
- Hydration and nutritional support
- Respiratory physiotherapy as needed
Complications of Streptococcal Pneumonia
If not promptly treated, streptococcal pneumonia may lead to:
- Empyema: Accumulation of pus in the pleural cavity
- Lung abscess
- Septicemia and shock
- Pericarditis
- Meningitis (especially in children and elderly)
- Respiratory failure
Prevention and Vaccination Strategies
Pneumococcal Vaccines
Two major types are recommended:
- PCV13 (Pneumococcal Conjugate Vaccine 13-valent)
- Used in children and high-risk adults
- PPSV23 (Pneumococcal Polysaccharide Vaccine 23-valent)
- For adults aged ≥65 years and those with chronic medical conditions
Both vaccines have significantly reduced the incidence of invasive pneumococcal disease.
Additional Preventive Measures
- Annual influenza vaccination to prevent secondary bacterial pneumonia
- Smoking cessation
- Managing underlying chronic diseases
- Good respiratory hygiene and handwashing
Prognosis and Outcomes
The prognosis of streptococcal pneumonia depends on:
- Timeliness of treatment initiation
- Patient’s age and immune status
- Presence of complications or comorbidities
With early and appropriate therapy, the majority of patients recover fully. However, in elderly or immunocompromised individuals, the mortality rate may reach 20–30%, especially with bacteremia or septic shock.
Streptococcal pneumonia remains a significant global health concern due to its potential severity and complications. Rapid diagnosis, appropriate antibiotic therapy, and preventive measures such as vaccination are essential in reducing its burden. Healthcare providers must remain vigilant for early signs, especially in high-risk populations, to ensure timely management and favorable outcomes.