Streptococcal peritonitis is an acute, life-threatening inflammation of the peritoneum caused by infection with Streptococcus species. While peritonitis can arise from various microbial agents, streptococcal involvement—particularly from Group A Streptococcus (GAS) and Group B Streptococcus (GBS)—is known for its aggressive clinical progression and high morbidity if not promptly managed. It may present as a primary (spontaneous) or secondary peritonitis depending on the origin of the infection.

Classification of Streptococcal Peritonitis
Primary Streptococcal Peritonitis
Occurs without an apparent source of intra-abdominal perforation. Most commonly seen in:
- Patients with cirrhosis and ascites (Spontaneous Bacterial Peritonitis, SBP)
- Children, particularly females, with underlying respiratory or skin infections
- Patients undergoing peritoneal dialysis (PD)
Secondary Streptococcal Peritonitis
Results from direct extension or perforation due to:
- Appendicitis
- Diverticulitis
- Bowel perforation
- Post-surgical infections
- Pelvic inflammatory disease
Pathophysiology and Bacterial Invasion
Streptococcal peritonitis occurs when streptococcal organisms breach the peritoneal cavity, triggering a severe immune response. The rapid multiplication of bacteria within the peritoneal fluid results in neutrophil activation, exudate formation, and in severe cases, systemic sepsis or multi-organ failure.
Causative Streptococcal Organisms
- Group A Streptococcus (GAS) – Streptococcus pyogenes
- Highly virulent; often associated with toxic shock syndrome
- Group B Streptococcus (GBS) – Streptococcus agalactiae
- Common in obstetric and gynecologic origins
- Streptococcus pneumoniae
- Often isolated in pediatric spontaneous peritonitis
- Streptococcus anginosus group
- Known for abscess formation within the abdominal cavity
Clinical Features of Streptococcal Peritonitis
The disease presents rapidly with signs of severe systemic and localized inflammation:
- Intense abdominal pain and tenderness
- Fever and chills
- Abdominal rigidity and guarding
- Nausea, vomiting, and ileus
- Hypotension and tachycardia (signs of sepsis)
- Altered mental status in severe systemic involvement
In patients with cirrhosis or on peritoneal dialysis, early signs may be subtle and require high clinical suspicion.
Diagnostic Workup
Physical Examination
- Abdominal distension, rebound tenderness, and signs of peritoneal irritation.
- In PD patients, dialysate fluid may appear cloudy with fibrin strands.
Laboratory Investigations
- CBC: Elevated WBC count with neutrophilia
- CRP and ESR: Markedly elevated
- Blood cultures: To detect systemic streptococcal infection
- Ascitic fluid analysis:
- PMN count > 250 cells/mm³
- Positive Gram stain or culture for Streptococcus spp.
- Decreased glucose and elevated lactate
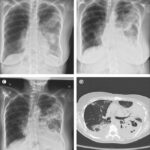
Imaging
- Ultrasound or CT scan of the abdomen:
- Ascites
- Intra-abdominal abscess
- Source identification in secondary peritonitis
Management and Antimicrobial Therapy
Empiric Antibiotic Therapy
Initiate broad-spectrum IV antibiotics immediately while awaiting culture results:
- Penicillin G or Ampicillin – First-line for streptococcal sensitivity
- Clindamycin – Inhibits streptococcal toxin production
- Third-generation cephalosporins (e.g., Cefotaxime) – For SBP
- Vancomycin – If resistant or mixed Gram-positive organisms suspected
Duration: Typically 10–14 days based on clinical response and source control.
Surgical and Supportive Measures
- Surgical intervention in secondary peritonitis for source control
- Perforation repair
- Drainage of abscess
- Peritoneal dialysis patients may require:
- Catheter removal in refractory cases
- Intraperitoneal antibiotic administration
- Fluid resuscitation, vasopressors, and ICU support for septic shock cases
Complications and Prognosis
Streptococcal peritonitis, if untreated or diagnosed late, can lead to:
- Septic shock
- Multi-organ failure
- Intra-abdominal abscesses
- Chronic peritoneal adhesions
- Mortality, especially in cirrhotic or immunocompromised individuals
Prompt treatment significantly reduces the fatality rate, especially in primary peritonitis.
Prevention and Risk Reduction Strategies
In Peritoneal Dialysis
- Strict aseptic technique during exchanges
- Proper catheter care
- Patient education on early signs of peritonitis
- Prophylactic antibiotics during procedures
In Cirrhosis
- Routine screening for spontaneous bacterial peritonitis
- Prophylactic antibiotics (e.g., Norfloxacin) in high-risk cases
- Management of ascites to reduce risk of infection
General Surgical Settings
- Early recognition and treatment of intra-abdominal infections
- Appropriate pre- and post-operative antibiotics
- Sterile surgical technique and drainage when needed
Streptococcal peritonitis is a serious infectious emergency that requires rapid clinical recognition, targeted antibiotic therapy, and, in many cases, surgical intervention. Whether spontaneous or secondary in origin, timely diagnosis and management are critical in reducing morbidity and mortality. Health professionals must be especially vigilant in high-risk populations such as peritoneal dialysis patients and individuals with cirrhosis. Continued awareness, early intervention, and preventive measures are essential to improving patient outcomes in this potentially fatal condition.