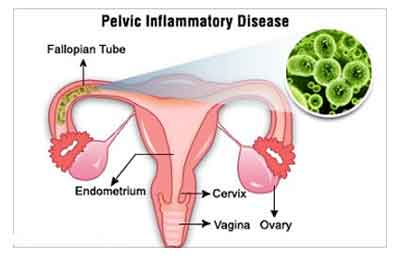
Streptococcal pelvic inflammatory disease (PID) is a severe form of reproductive tract infection caused by Streptococcus species, notably Group A Streptococcus (GAS) and Group B Streptococcus (GBS). Though PID is typically associated with sexually transmitted pathogens like Neisseria gonorrhoeae and Chlamydia trachomatis, streptococcal PID presents unique clinical challenges due to its aggressive progression and potential for systemic involvement.
Pathogenesis: How Streptococcus Causes PID
Streptococcal PID arises when Streptococcus bacteria ascend from the lower genital tract into the uterus, fallopian tubes, and adjacent pelvic structures. Entry points often include:
- Postpartum period
- Post-abortion procedures
- Intrauterine device (IUD) insertion
- Gynecological surgery or instrumentation
The bacterial invasion leads to acute inflammation, tissue necrosis, and the risk of abscess formation or peritonitis.
Causative Agents: Streptococcal Species in PID
Group A Streptococcus (Streptococcus pyogenes)
- Highly invasive and toxin-producing
- Rapid onset of symptoms and higher systemic risk
Group B Streptococcus (Streptococcus agalactiae)
- Commonly colonizes the vaginal tract
- Often implicated in postpartum and post-procedural PID
- Can affect neonates if not treated in mothers
Other species such as Streptococcus anginosus may be involved in polymicrobial pelvic abscesses.
Clinical Presentation and Symptoms
Streptococcal PID often exhibits an abrupt and severe symptom profile:
- Lower abdominal and pelvic pain
- Fever (>38.5°C) and chills
- Purulent vaginal discharge
- Dyspareunia (painful intercourse)
- Dysuria (painful urination)
- Adnexal tenderness on pelvic exam
- Uterine or cervical motion tenderness
Systemic signs of streptococcal infection such as hypotension, tachycardia, or toxic shock may indicate invasive disease requiring urgent care.
Diagnostic Evaluation
Pelvic Examination
- Bimanual exam reveals uterine and adnexal tenderness.
- Cervical motion tenderness is a hallmark of PID.
Laboratory Tests
- Complete blood count (CBC): Elevated white blood cells
- C-reactive protein (CRP) and ESR: Elevated inflammatory markers
- Vaginal and cervical swabs: Culture and sensitivity testing for Streptococcus species
- Blood cultures: Essential in cases of suspected invasive streptococcal disease
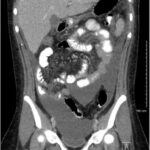
Imaging
- Transvaginal ultrasound: Detects tubo-ovarian abscess, free fluid, or thickened fallopian tubes
- CT or MRI: Reserved for complicated or atypical presentations
Treatment Strategies for Streptococcal PID
Empirical Antimicrobial Therapy
Immediate initiation of broad-spectrum antibiotics is crucial. For streptococcal PID, regimens typically include:
- IV Clindamycin + Gentamicin for broad anaerobic and streptococcal coverage
- Penicillin G for confirmed Group A or B Streptococcus
- Ampicillin-Sulbactam as an alternative in polymicrobial cases
Duration: 10–14 days, with transition to oral antibiotics upon clinical improvement.
Surgical Intervention
Indications include:
- Failure to respond to medical therapy
- Drainage of tubo-ovarian abscess
- Removal of necrotic tissue in cases of severe sepsis or necrotizing fasciitis
Complications and Prognosis
Untreated or inadequately treated streptococcal PID may result in:
- Tubo-ovarian abscess
- Pelvic peritonitis
- Infertility due to tubal damage
- Chronic pelvic pain
- Septic shock and multi-organ failure
Mortality increases significantly in invasive Streptococcus pyogenes infections, highlighting the need for rapid recognition and treatment.
Epidemiology and Risk Factors
While streptococcal PID is relatively rare compared to other etiologies, its incidence is rising due to increased invasive streptococcal disease globally. High-risk groups include:
- Postpartum and post-abortion women
- Patients with IUDs
- Individuals with recent gynecologic surgeries
- Immunocompromised women
Preventive measures such as infection control during procedures and routine GBS screening in pregnancy are critical.
Prevention and Patient Education
Screening and Prophylaxis
- GBS screening in pregnant women with intrapartum prophylaxis
- Aseptic technique during gynecological procedures
- Early treatment of vaginal or urinary tract infections
Patient Awareness
- Recognize early signs of pelvic infection
- Avoid self-medication
- Seek immediate care for post-procedural fevers or pain
Streptococcal pelvic inflammatory disease is a serious and potentially life-threatening condition requiring timely diagnosis, aggressive antibiotic therapy, and careful follow-up. Clinicians must maintain a high index of suspicion in post-procedural or postpartum patients presenting with signs of pelvic infection. Through vigilant prevention, accurate diagnosis, and swift treatment, the complications of this invasive infection can be significantly minimized.