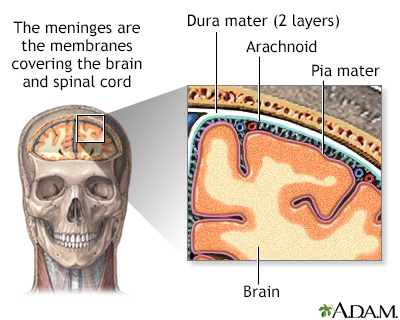
Streptococcal meningitis is a life-threatening bacterial infection characterized by the inflammation of the protective membranes covering the brain and spinal cord, known as the meninges. It is primarily caused by various strains of Streptococcus bacteria, including Streptococcus pneumoniae and Streptococcus agalactiae (Group B Streptococcus). This condition can progress rapidly and requires immediate medical intervention.
Causes and Risk Factors of Streptococcal Meningitis
Primary Causative Agents
- Streptococcus pneumoniae: The most common cause in adults and older children. It often follows pneumonia, sinusitis, or otitis media.
- Group B Streptococcus (GBS): A major cause in neonates, typically transmitted from mother to child during childbirth.
- Streptococcus pyogenes (Group A Streptococcus): Less common but highly virulent.
Risk Factors
- Age extremes: neonates and elderly individuals
- Immunosuppression (HIV, chemotherapy, splenectomy)
- Skull trauma or neurosurgical procedures
- Chronic conditions: diabetes mellitus, alcoholism
- Cochlear implants or CSF leaks
Symptoms of Streptococcal Meningitis
Streptococcal meningitis manifests with both general and neurological symptoms that escalate rapidly:
- High fever and chills
- Severe headache
- Neck stiffness
- Photophobia (sensitivity to light)
- Nausea and vomiting
- Seizures
- Altered mental status or confusion
- Lethargy or coma in severe cases
In infants:
- Poor feeding
- Irritability
- Bulging fontanelle
- Hypotonia
Pathophysiology: How Infection Develops
The infection usually begins with the colonization of the respiratory tract or genitourinary tract. Once the bacteria breach mucosal barriers, they enter the bloodstream and penetrate the blood-brain barrier (BBB), initiating a potent inflammatory response in the CNS.
Diagnostic Methods for Streptococcal Meningitis
Lumbar Puncture (Spinal Tap)
- CSF Analysis: Elevated opening pressure, neutrophilic pleocytosis, decreased glucose, elevated protein.
- Gram Stain: Often reveals Gram-positive cocci in chains.
- CSF Culture: Gold standard for confirming the causative organism.
Additional Tests
- Blood cultures to identify bacteremia.
- CT or MRI to rule out brain abscess, increased intracranial pressure, or hydrocephalus.
- PCR testing and antigen detection for rapid diagnosis.
Treatment Protocols for Streptococcal Meningitis
Empiric Antibiotic Therapy
Initiate treatment immediately, even before culture results, using:
- Ceftriaxone or Cefotaxime + Vancomycin
- Add Ampicillin in neonates or elderly to cover Listeria
- Modify based on culture and sensitivity
Duration of Therapy
- 10–14 days for uncomplicated S. pneumoniae
- 14–21 days for GBS or complicated cases
Adjunctive Therapy
- Dexamethasone administered before or with the first dose of antibiotics to reduce inflammatory damage, especially in pneumococcal meningitis.
Supportive Care
- Intravenous fluids, oxygen, antipyretics
- Monitoring of intracranial pressure
- Management of seizures with anticonvulsants
Complications and Prognosis
Despite treatment, streptococcal meningitis can lead to severe complications:
- Neurological deficits (hearing loss, cognitive impairment)
- Sepsis and septic shock
- Hydrocephalus
- Cerebral edema
- Death, especially if diagnosis and treatment are delayed
Prognosis varies based on age, immune status, timeliness of treatment, and strain virulence. Mortality ranges from 10–30%, higher in pneumococcal cases.
Prevention Strategies
Vaccination
- Pneumococcal Conjugate Vaccine (PCV13) and Polysaccharide Vaccine (PPSV23): Reduce risk of S. pneumoniae infection.
- Maternal screening and intrapartum antibiotic prophylaxis for GBS in pregnant women.
Infection Control
- Prompt treatment of otitis media, sinus infections
- Avoidance of contact with infected individuals
- Strict hygiene during childbirth and neonatal care
Epidemiology and Global Impact
Streptococcal meningitis contributes significantly to the global burden of meningitis, especially in:
- Sub-Saharan Africa’s meningitis belt
- Neonatal populations in developing countries
- Immunocompromised populations worldwide
According to WHO estimates, bacterial meningitis causes over 250,000 deaths annually, with Streptococcus pneumoniae being a leading culprit.
Streptococcal meningitis remains a critical medical emergency with high mortality and morbidity rates. Early recognition, prompt antibiotic treatment, and effective prevention strategies—including vaccination and perinatal care—are essential to reduce the global burden of this condition. Continuous surveillance and medical advancements remain vital in combating its devastating impact on public health.