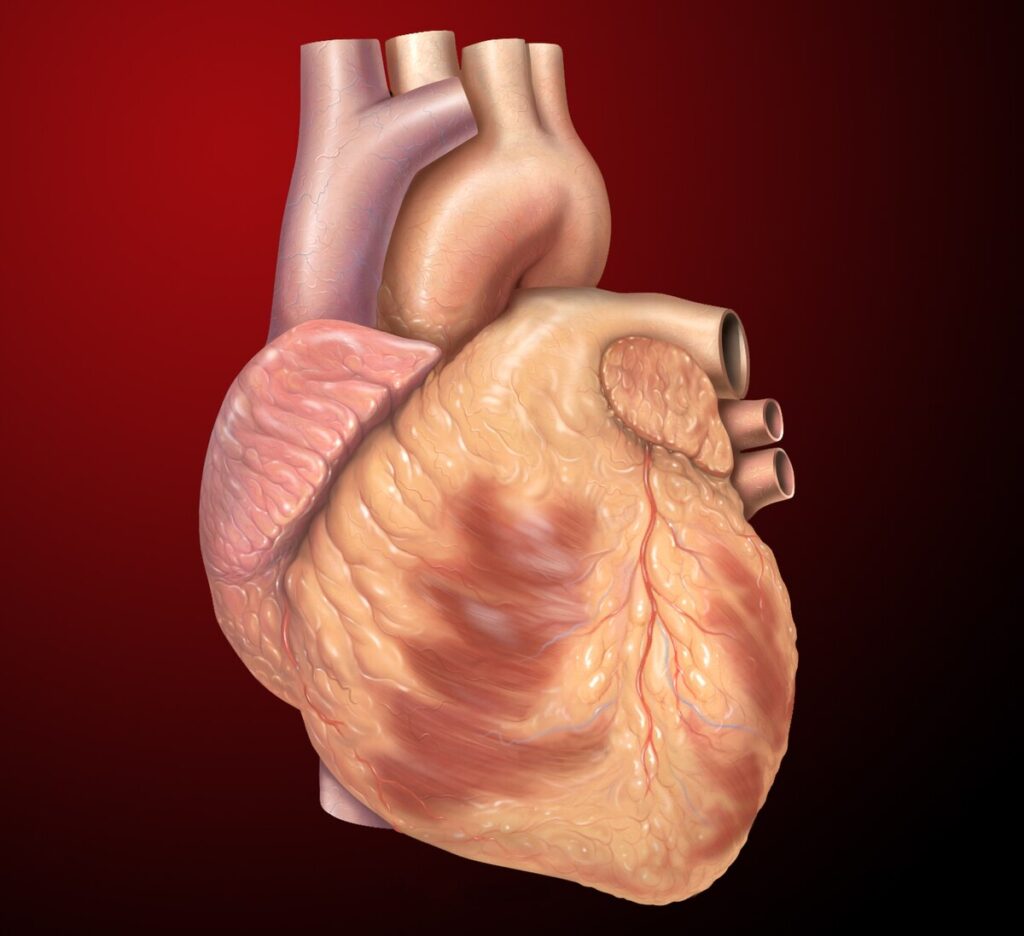
Carditis refers to the inflammation of the heart, which can affect one or more of its layers: the myocardium (heart muscle), pericardium (outer lining), or endocardium (inner lining). This condition may arise due to infections, autoimmune diseases, or other medical factors, and it poses serious risks if left untreated. Early diagnosis and appropriate management are crucial for preventing complications.
Types of Carditis
1. Myocarditis
Myocarditis is the inflammation of the heart muscle. It can impair the heart’s ability to pump blood, potentially leading to heart failure. Common causes include viral infections, autoimmune disorders, and exposure to toxins.
Symptoms:
- Chest pain
- Fatigue
- Shortness of breath
- Irregular heartbeats
Causes:
- Viral infections (e.g., Coxsackievirus, adenovirus)
- Autoimmune diseases (e.g., lupus)
- Medications and toxins
2. Pericarditis
Pericarditis involves inflammation of the pericardium, the thin sac surrounding the heart. This type can lead to complications such as pericardial effusion.
Symptoms:
- Sharp chest pain that worsens when lying down
- Fever
- Palpitations
Causes:
- Viral and bacterial infections
- Trauma
- Chronic diseases (e.g., kidney failure)
3. Endocarditis
Endocarditis is the inflammation of the heart’s inner lining, often caused by bacterial or fungal infections. It primarily affects individuals with pre-existing heart conditions.
Symptoms:
- Fever and chills
- Fatigue
- Heart murmurs
- Blood in urine
Causes:
- Bacterial infections (e.g., Streptococcus, Staphylococcus)
- Fungal infections
- Intravenous drug use
Causes and Risk Factors
Carditis can result from various factors, including:
- Infections: Viruses, bacteria, fungi, or parasites.
- Autoimmune Diseases: Conditions like rheumatoid arthritis or lupus.
- Medications: Certain drugs, including chemotherapy agents.
- Radiation Therapy: Used in cancer treatment.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and substance abuse.
Diagnosis of Carditis
Diagnosing carditis involves a combination of clinical evaluation and diagnostic tests:
- Physical Examination: Listening for heart murmurs or friction rubs.
- Blood Tests: To detect infections or markers of inflammation.
- Imaging:
- Echocardiogram: Assesses heart structure and function.
- MRI: Identifies inflammation and tissue damage.
- X-Ray: Checks for fluid around the heart.
- Electrocardiogram (ECG): Detects abnormal heart rhythms.
- Biopsy: Rarely, a tissue sample may be taken for detailed analysis.
Treatment Options
Medications
- Antibiotics or Antifungals: For infections.
- Anti-inflammatory Drugs: NSAIDs or corticosteroids to reduce inflammation.
- Immunosuppressants: For autoimmune-related carditis.
Procedures
- Pericardiocentesis: Removes excess fluid from the pericardium.
- Surgery: Valve repair or replacement for severe endocarditis.
Lifestyle Modifications
- Rest and avoiding strenuous activities.
- Smoking cessation and alcohol moderation.
- Heart-healthy diet rich in fruits, vegetables, and lean proteins.
Prevention
Preventive measures can significantly reduce the risk of carditis:
- Vaccinate against infections such as influenza and COVID-19.
- Practice good hygiene to prevent bacterial infections.
- Manage chronic conditions like diabetes and hypertension.
- Regular medical checkups, especially if you have a history of heart disease.
Prognosis and Long-Term Outlook
The outcome of carditis depends on its type, severity, and the promptness of treatment. Many individuals recover fully with timely care, but complications like chronic heart disease or arrhythmias may arise in severe cases.