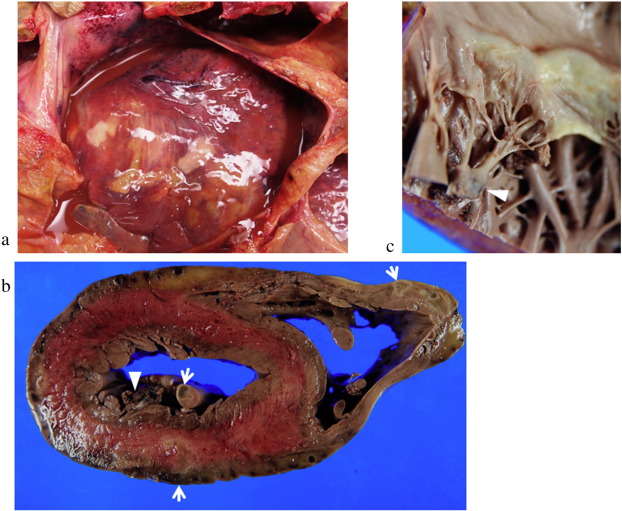
Streptococcal endocarditis is a severe form of infective endocarditis caused by Streptococcus species, most commonly the viridans group streptococci (VGS). This condition involves the infection of the endocardium, the inner lining of the heart chambers and valves, typically affecting damaged or prosthetic heart valves. Without timely treatment, streptococcal endocarditis can lead to valve destruction, systemic embolism, and death.
This infection remains a significant cardiovascular threat, particularly in patients with congenital heart defects, rheumatic heart disease, or prosthetic valves.
Causative Organisms and Risk Factors
Common Streptococcus Species Involved
- Streptococcus viridans group (e.g., S. mitis, S. sanguinis, S. mutans)
- Streptococcus bovis (linked to gastrointestinal malignancies)
- Streptococcus pyogenes (rarely, in acute cases)
Risk Factors
| Category | Details |
|---|---|
| Cardiac | Congenital heart disease, prosthetic heart valves, prior endocarditis |
| Procedural | Dental procedures, gastrointestinal endoscopy |
| Infectious | Bacteremia from poor dental hygiene, intravenous drug use |
| Systemic | Immunosuppression, malignancy, chronic kidney disease |
Pathogenesis of Streptococcal Endocarditis
The development of streptococcal endocarditis requires:
- Endothelial damage to the cardiac valve or endocardium.
- Platelet-fibrin deposition at the site of injury.
- Bacteremia, allowing streptococci to adhere to the thrombus.
- Vegetation formation, where bacteria proliferate and evade immune clearance.
These vegetations may fragment and embolize, affecting the lungs, brain, kidneys, or spleen.
Clinical Presentation
General Symptoms
- Persistent fever
- Chills and night sweats
- Malaise, fatigue, and weight loss
- Anorexia
Cardiac and Embolic Manifestations
- New or changing heart murmur
- Congestive heart failure in advanced stages
- Embolic stroke, splenic infarcts, renal infarctions
- Janeway lesions, Osler nodes, Roth spots, and splinter hemorrhages as classic signs
Subacute vs Acute Presentation
| Form | Characteristics |
|---|---|
| Subacute | Low-grade fever, indolent course, common with S. viridans |
| Acute | High fever, rapid progression, typically S. aureus but can rarely be streptococcal |
Diagnostic Criteria for Streptococcal Endocarditis
Modified Duke Criteria
Major Criteria:
- Positive blood cultures for Streptococcus viridans or S. bovis
- Evidence of endocardial involvement (echocardiogram showing vegetations)
Minor Criteria:
- Predisposing heart condition or IV drug use
- Fever ≥ 38°C
- Vascular phenomena (e.g., emboli, Janeway lesions)
- Immunologic phenomena (e.g., glomerulonephritis, Osler nodes)
- Positive blood cultures not meeting major criteria
Diagnosis is confirmed by:
- 2 major
- 1 major + 3 minor
- 5 minor criteria
Investigations
| Test | Purpose |
|---|---|
| Blood cultures (multiple sets) | Essential for identifying streptococcal species |
| Echocardiography (TEE preferred) | Detects vegetations, abscesses, and valve perforation |
| CBC and Inflammatory Markers | Leukocytosis, elevated ESR/CRP |
| Urinalysis | Microscopic hematuria (due to emboli or immune complexes) |
Treatment Protocols for Streptococcal Endocarditis
Antibiotic Therapy
Treatment is tailored based on antibiotic susceptibility, with the goal of sterilizing vegetations and preventing complications.
Native Valve Endocarditis by Penicillin-Susceptible Streptococci
- Penicillin G IV or Ceftriaxone IV for 4 weeks
- Alternative: Vancomycin IV for patients with β-lactam allergy
Prosthetic Valve Endocarditis
- Penicillin G + Gentamicin for synergistic effect (6 weeks)
- Monitor for nephrotoxicity and ototoxicity with aminoglycosides
Penicillin-Resistant Strains
- High-dose penicillin or ceftriaxone + gentamicin
- Consider vancomycin if MIC > 0.5 µg/mL
Surgical Intervention
Indications for surgery include:
- Heart failure due to valve dysfunction
- Persistent bacteremia despite antibiotics
- Large vegetations (>10 mm) with embolic risk
- Valve perforation or abscess formation
- Prosthetic valve dehiscence
Prognosis and Complications
Complications
- Valvular destruction and regurgitation
- Heart failure
- Embolic stroke or infarcts
- Mycotic aneurysms
- Immune complex glomerulonephritis
Prognosis
| Factor | Effect |
|---|---|
| Early diagnosis | Improved survival |
| Prosthetic valve involvement | Higher mortality risk |
| Streptococcus viridans infection | Better prognosis than S. aureus |
| Prompt surgical management | Reduces risk of heart failure and embolism |
Prevention Strategies
Prophylactic Antibiotics
Recommended for high-risk patients undergoing dental or invasive procedures, particularly those with:
- Prosthetic heart valves
- History of infective endocarditis
- Certain congenital heart diseases
Amoxicillin 2g orally 30–60 minutes before procedure is the standard regimen. Alternatives include clindamycin or azithromycin in penicillin-allergic individuals.
Oral Hygiene
- Maintaining excellent dental care is crucial in reducing bacteremia risk.
- Regular dental check-ups are essential for high-risk individuals.
Frequently Asked Questions:
What is streptococcal endocarditis?
It is an infection of the inner lining of the heart caused by Streptococcus bacteria, often affecting damaged heart valves.
How is it diagnosed?
Diagnosis is made using blood cultures, echocardiography, and criteria such as the Modified Duke Criteria.
Can streptococcal endocarditis be cured?
Yes. With timely and appropriate antibiotic therapy, often combined with surgery, most cases are curable.
Is streptococcal endocarditis contagious?
No. The condition itself is not contagious, though the bacteria may be part of the normal flora in the mouth or gut.
What are the chances of recurrence?
Recurrence risk is higher in patients with incomplete treatment, underlying heart disease, or poor oral hygiene.
Streptococcal endocarditis remains a life-threatening condition that requires rapid diagnosis, effective antimicrobial therapy, and sometimes surgical intervention. With advances in imaging, microbiology, and cardiac surgery, the outlook has significantly improved, particularly when managed by a multidisciplinary team. Preventive strategies, especially in high-risk individuals, remain a cornerstone of reducing incidence and recurrence.