Strabismus, commonly referred to as crossed eyes or eye misalignment, is a condition in which the eyes do not properly align with each other when looking at an object. One eye may turn inwards, outwards, upwards, or downwards, while the other eye remains focused. This misalignment interferes with binocular vision, leading to double vision or suppression of one eye by the brain.
Strabismus can be constant or intermittent, congenital or acquired, and may present at any age. Prompt evaluation and treatment are crucial to preserve vision and prevent complications such as amblyopia (lazy eye).
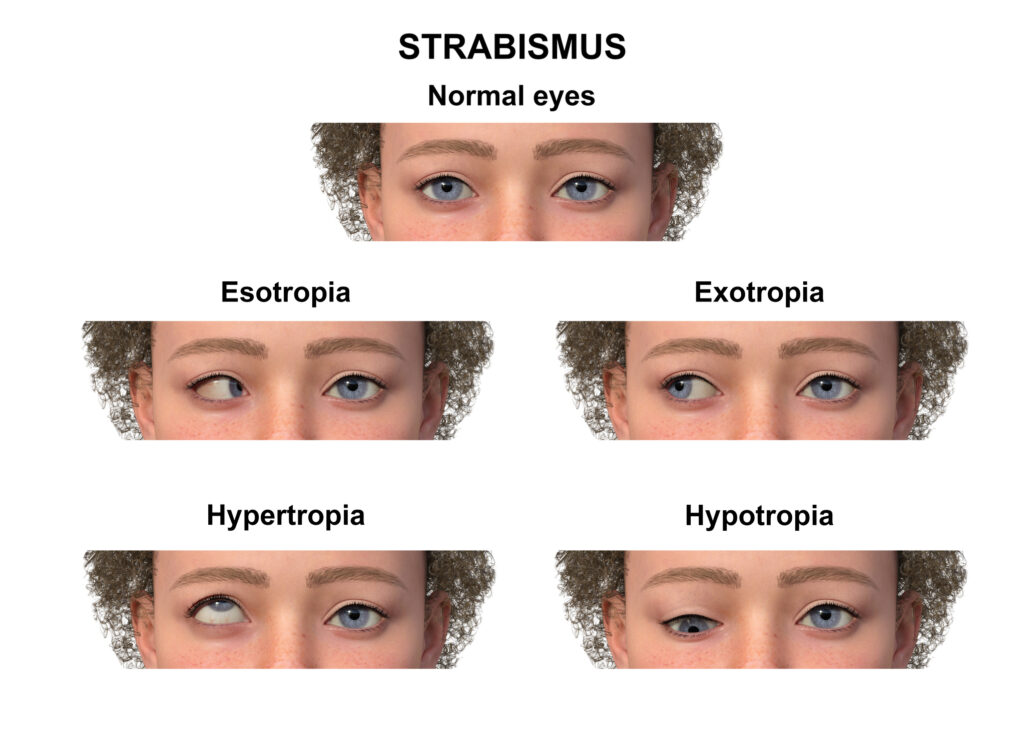
Types of Strabismus
Esotropia (Inward Turning of the Eye)
- Most commonly diagnosed form in infants and young children.
- The eye turns toward the nose.
- May be congenital or acquired (accommodative esotropia).
Exotropia (Outward Turning of the Eye)
- More commonly intermittent than constant.
- The eye turns away from the nose.
- Often observed when the patient is tired, daydreaming, or looking into the distance.
Hypertropia and Hypotropia
- Vertical misalignment:
- Hypertropia: One eye turns upward.
- Hypotropia: One eye turns downward.
- Typically caused by cranial nerve palsies, trauma, or thyroid eye disease.
Paralytic and Restrictive Strabismus
- Result from nerve damage or mechanical restrictions:
- Paralytic (e.g., CN III, IV, VI palsy)
- Restrictive (e.g., orbital trauma, thyroid orbitopathy)
Causes and Risk Factors
Strabismus may develop due to various neuromuscular, genetic, or structural causes. Key contributing factors include:
| Category | Examples |
|---|---|
| Congenital | Genetic predisposition, brain development disorders |
| Neurological | Cerebral palsy, brain tumors, hydrocephalus |
| Refractive | Uncorrected hyperopia (farsightedness) |
| Muscle dysfunction | Abnormal eye muscle tone or control |
| Systemic diseases | Down syndrome, stroke, thyroid dysfunction |
| Trauma | Orbital fractures, cranial nerve damage |
Symptoms of Strabismus
Patients may experience both visual and physical symptoms, including:
- Misalignment of the eyes
- Double vision (diplopia)
- Head tilting or turning
- Eye strain and fatigue
- Loss of depth perception
- Difficulty with reading or focusing
- Squinting or closing one eye in bright light
In children, the brain often suppresses input from the misaligned eye, resulting in amblyopia, which requires early intervention.
Pathophysiology of Strabismus
Strabismus is primarily a neuromuscular control issue affecting the extraocular muscles. Each eye is controlled by six muscles, and proper coordination is essential for binocular vision.
Dysfunction in these nerves or their corresponding muscles disrupts alignment, resulting in strabismus.
Diagnosis of Strabismus
Clinical Evaluation
A comprehensive eye exam is vital, including:
- Visual acuity test
- Cover test (to detect hidden deviations)
- Hirschberg test (light reflex test)
- Ocular motility exam
- Retinal exam (to rule out retinal disease)
- Cycloplegic refraction (to assess refractive error)
Additional Tests
- Prism cover test: Quantifies the angle of deviation.
- MRI/CT scan: If neurologic or structural abnormalities are suspected.
- Synoptophore: Measures binocular function and angle of strabismus.
Treatment Options for Strabismus
1. Eyeglasses and Corrective Lenses
- Effective for refractive strabismus, especially accommodative esotropia.
- Prescription glasses reduce the demand on eye muscles.
2. Vision Therapy
- Non-surgical approach using eye exercises to improve coordination.
- Often used in intermittent exotropia and post-operative care.
3. Prism Lenses
- Redirect light entering the eye to compensate for mild deviations.
- Beneficial for patients with diplopia and minor misalignments.
4. Patching Therapy
- Used to treat amblyopia by covering the dominant eye.
- Encourages the brain to utilize the weaker eye for visual development.
5. Strabismus Surgery
- Reserved for cases unresponsive to non-surgical methods.
- Involves tightening, weakening, or repositioning eye muscles.
| Procedure | Purpose |
|---|---|
| Recession | Weakens an overacting muscle |
| Resection | Strengthens a weak muscle |
| Adjustable sutures | Allows postoperative fine-tuning of alignment |
Success rates are high, but some patients may require reoperation or continued therapy.
Complications and Risks
Untreated or improperly managed strabismus can lead to:
- Permanent vision loss in the weaker eye (amblyopia)
- Social or psychological impact due to visible misalignment
- Reduced depth perception
- Diplopia in adults post-surgery
- Head posture problems from chronic eye misalignment
Prognosis and Long-Term Outcomes
With early detection and appropriate treatment, most children achieve normal vision and eye alignment. Adult outcomes vary depending on the underlying cause, chronicity, and response to intervention. Regular follow-up is essential to monitor progress and prevent regression.
Strabismus in Adults
While often considered a pediatric issue, adult-onset strabismus may result from:
- Cranial nerve palsies
- Stroke or trauma
- Graves’ orbitopathy
- Brain tumors
Management may include prism therapy, Botox injections, or surgery. Accurate diagnosis is critical to address secondary causes and prevent further neurologic damage.
Frequently Asked Questions:
Can strabismus correct itself?
Some mild cases in infants resolve spontaneously, but persistent strabismus generally requires medical intervention.
Is strabismus hereditary?
Yes, there is a genetic predisposition, especially in congenital cases.
What age is best for strabismus surgery?
Early intervention (typically before age 2–4) improves binocular development and prevents amblyopia.
Can adults with strabismus be treated?
Absolutely. Adults may benefit from surgery, prisms, or vision therapy, depending on the cause and severity.
Is strabismus the same as lazy eye?
No. Strabismus refers to eye misalignment, while amblyopia (lazy eye) is reduced vision in an eye that is otherwise structurally normal.
Strabismus represents a complex interplay of neuromuscular, structural, and refractive abnormalities affecting eye alignment and vision. Early and accurate diagnosis, combined with a customized treatment plan, can dramatically improve visual outcomes and quality of life. Whether through glasses, therapy, or surgery, restoring proper alignment is not merely cosmetic—it is essential for functional, binocular vision.