Staphylococcus saprophyticus is a coagulase-negative, gram-positive bacterium responsible for a significant proportion of urinary tract infections (UTIs), particularly in sexually active young women. Unlike Escherichia coli, which dominates UTI cases overall, S. saprophyticus accounts for approximately 5–20% of community-acquired UTIs. It is notable for its urease production, adherence to uroepithelial cells, and resistance to urinary flushing, which contribute to its uropathogenicity.
Microbiological Characteristics of S. saprophyticus
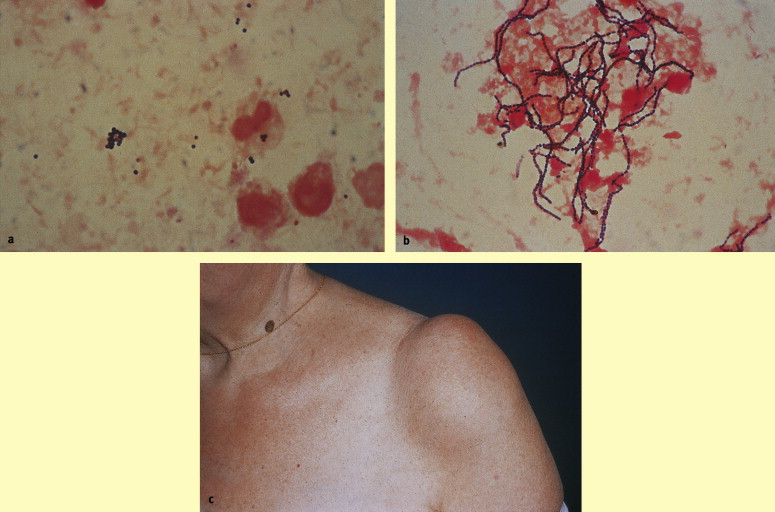
- Gram-positive cocci arranged in clusters
- Coagulase-negative and novobiocin-resistant
- Urease-positive, contributing to urine alkalinization
- Non-hemolytic on blood agar
- Natural inhabitant of the gastrointestinal tract, genitourinary tract, and perineum
This organism is distinct from other staphylococci due to its ability to thrive in the urinary tract environment and its preference for young female hosts.
Virulence Factors
| Virulence Factor | Function |
|---|---|
| Urease | Converts urea into ammonia, raises pH |
| Adhesins | Mediate binding to uroepithelial cells |
| Surface proteins | Enhance persistence in urinary tract |
| Biofilm formation | Increases resistance to host defenses |
Epidemiology and Risk Factors
Population Affected
- Sexually active females, particularly those aged 15–30
- Women using spermicides or diaphragms
- Patients with recurrent UTIs
- Individuals with poor perineal hygiene
Seasonal Pattern
Infections by S. saprophyticus exhibit a higher incidence during late summer and early fall, a pattern not observed with other uropathogens.
Clinical Presentation of S. saprophyticus UTI
Common Symptoms
- Dysuria (painful urination)
- Urinary frequency and urgency
- Suprapubic pain
- Cloudy or malodorous urine
- Hematuria (less common)
- Absence of fever in uncomplicated cystitis
Symptoms are often indistinguishable from UTIs caused by E. coli, but S. saprophyticus typically causes milder infections with lower risk of pyelonephritis.
Diagnostic Evaluation
Laboratory Investigations
| Test | Finding |
|---|---|
| Urinalysis | Pyuria, bacteriuria, possible hematuria |
| Urine Culture | >10⁵ CFU/mL of S. saprophyticus |
| Gram Stain | Gram-positive cocci in clusters |
| Novobiocin Sensitivity Test | Resistance confirms S. saprophyticus |
It is essential to distinguish S. saprophyticus from other coagulase-negative staphylococci that are typically contaminants, especially in women presenting with classic UTI symptoms.
Differential Diagnosis
| Condition | Key Distinguishing Feature |
|---|---|
| E. coli UTI | More common, often with more severe symptoms |
| Enterococcus faecalis UTI | Gram-positive cocci but bile esculin positive |
| Vaginitis or urethritis | Often associated with vaginal discharge or irritation |
| Interstitial cystitis | Chronic symptoms without bacterial growth |
Antimicrobial Therapy for S. saprophyticus UTI
First-Line Treatment
| Antibiotic | Dose | Duration |
|---|---|---|
| Nitrofurantoin | 100 mg BID | 5 days |
| Trimethoprim-Sulfamethoxazole | 160/800 mg BID | 3 days |
| Fosfomycin | 3 g single dose | Single dose |
Alternative Options
- Amoxicillin-clavulanate or cephalexin in pregnancy
- Fluoroquinolones (e.g., ciprofloxacin) only when first-line agents fail due to resistance concerns
S. saprophyticus is generally susceptible to a wide range of oral antibiotics, but emerging resistance to trimethoprim has been noted in some regions.
Complications of Untreated S. saprophyticus UTI
- Ascending infection leading to pyelonephritis (rare)
- Recurrent urinary tract infections
- Bladder wall inflammation and discomfort
- Potential bacteremia in immunocompromised hosts
Prompt treatment ensures rapid symptom resolution and prevention of recurrence.
Prevention Strategies
Behavioral Modifications
- Urinate after sexual intercourse
- Maintain proper perineal hygiene
- Avoid spermicide use if recurrent UTIs occur
- Increase fluid intake to flush urinary tract
Prophylactic Antibiotics
For patients with recurrent infections, low-dose prophylaxis or post-coital antibiotic use may be considered under medical supervision.
Summary Table: Key Points on S. saprophyticus UTI
| Aspect | Details |
|---|---|
| Organism | Staphylococcus saprophyticus |
| Common Population | Sexually active women (15–30 years) |
| Virulence | Urease production, adhesins, biofilm |
| Diagnosis | Culture with novobiocin resistance |
| Treatment | Nitrofurantoin, TMP-SMX, Fosfomycin |
| Prevention | Hygiene, post-coital voiding, avoid spermicides |
Staphylococcus saprophyticus is a significant cause of uncomplicated urinary tract infections, especially among young women. Its identification through culture and novobiocin resistance testing is critical for accurate diagnosis and treatment. While generally responsive to first-line oral antibiotics, prevention of recurrence relies heavily on behavioral practices and, in select cases, prophylactic therapy. Vigilant clinical management ensures rapid resolution and minimizes complications.