Staphylococcus peritonitis refers to inflammation of the peritoneum caused by Staphylococcus species, notably Staphylococcus aureus and coagulase-negative staphylococci. It frequently arises in patients undergoing peritoneal dialysis (PD), particularly continuous ambulatory peritoneal dialysis (CAPD), and carries a significant risk for morbidity, technique failure, and hospitalization. Methicillin-resistant S. aureus (MRSA) presents additional challenges due to limited therapeutic options and increased virulence.
Etiology and Microbiological Profile
Common Causative Pathogens
- Staphylococcus aureus: Most virulent; causes purulent, rapidly progressing peritonitis.
- Coagulase-negative Staphylococci (e.g., S. epidermidis): Frequently associated with catheter-related infections; more indolent course.
- MRSA: Associated with nosocomial outbreaks and higher complication rates.
Risk Factors for Staphylococcus Peritonitis
| Risk Factor | Description |
|---|---|
| Peritoneal dialysis (CAPD/CCPD) | Direct access to the peritoneum increases infection risk |
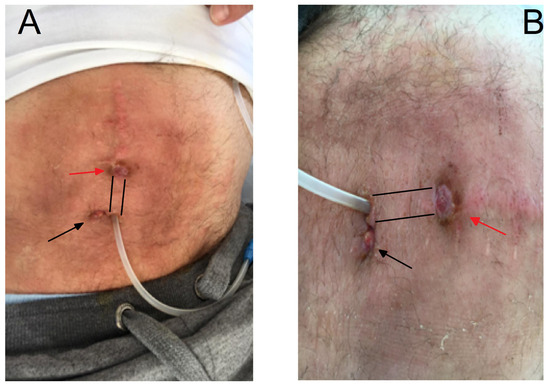
| Poor catheter hygiene or technique errors | Major cause of bacterial inoculation |
| Exit-site or tunnel infections | Precursor to peritonitis in many cases |
| Nasal or skin carriage of S. aureus | Increases likelihood of endogenous infection |
| Immunocompromised state | Reduces host defense against staphylococcal invasion |
| Recurrent episodes of peritonitis | Weakens local immune response and peritoneal integrity |
Clinical Manifestations
Signs and Symptoms
- Cloudy peritoneal dialysate (hallmark feature)
- Abdominal pain and tenderness
- Fever and chills
- Nausea and vomiting
- Generalized malaise
- Rebound tenderness in severe cases
Peritoneal Dialysis Fluid Analysis
- WBC count >100 cells/μL (typically >50% neutrophils)
- Gram stain may reveal gram-positive cocci in clusters
- Culture on blood agar and selective media confirms S. aureus or MRSA
Diagnostic Approach
Essential Investigations
| Test | Purpose |
|---|---|
| Dialysate cell count | Confirms inflammatory process |
| Gram stain and culture of effluent | Identifies organism and guides antibiotic therapy |
| Blood cultures (if febrile) | Rules out systemic dissemination |
| Nasal swab for MRSA screening | Identifies colonization source |
| Imaging (ultrasound/CT abdomen) | Detects intra-abdominal abscess or catheter complications |
Differential Diagnosis
| Condition | Distinguishing Features |
|---|---|
| Gram-negative peritonitis | More severe systemic symptoms, often linked to bowel perforation |
| Fungal peritonitis | Refractory to standard antibiotics, slower onset |
| Tuberculous peritonitis | Subacute onset, associated with ascites, weight loss |
| Chemical peritonitis | No infectious source; related to irritants in dialysis fluid |
Treatment of Staphylococcus Peritonitis
Empiric Antimicrobial Therapy
Initial therapy should cover both gram-positive and gram-negative organisms until culture results are available:
- Vancomycin (15–20 mg/kg IV or intraperitoneal) every 5–7 days for MRSA
- First-generation cephalosporins (e.g., cefazolin) for MSSA
- Add third-generation cephalosporin or aminoglycoside if gram-negative organisms are also suspected
Directed Therapy Based on Culture Results
| Organism | Recommended Antibiotic | Duration |
|---|---|---|
| MSSA | Cefazolin or Nafcillin | 14–21 days |
| MRSA | Vancomycin or Linezolid | 21 days |
| CoNS | Vancomycin or Cefazolin (if sensitive) | 14 days |
Route: Intraperitoneal administration is preferred due to higher local concentrations and faster bacterial clearance.
Catheter Management
Retention vs. Removal
- Retain Catheter: If early response within 48–72 hours of therapy and no tunnel/exit-site infection.
- Remove Catheter: If relapse, refractory infection, or concurrent exit-site/tunnel infection by S. aureus or MRSA.
Catheter replacement can be considered after 2–3 weeks of infection-free status, depending on patient stability.
Complications of Staphylococcus Peritonitis
| Complication | Description |
|---|---|
| Peritoneal membrane failure | Leads to technique failure and transfer to hemodialysis |
| Relapsing or refractory infection | Suggests biofilm formation or inadequate source control |
| Intra-abdominal abscess | May require surgical drainage |
| Septicemia | Particularly in MRSA cases with hematogenous spread |
| Mortality | Higher in elderly and immunocompromised patients |
Infection Prevention Strategies
For Patients on Peritoneal Dialysis
- Strict aseptic technique during bag exchange
- Topical mupirocin or gentamicin ointment at catheter exit-site
- Decolonization therapy for nasal S. aureus carriers
- Routine screening and retraining on exchange procedures
- Prompt treatment of exit-site infections
Prognosis and Outcome
The outcome of staphylococcus peritonitis depends on the following factors:
- Timely initiation of appropriate antibiotics
- Methicillin susceptibility of the organism
- Catheter management decisions
- Presence of complications such as abscess or systemic spread
MSSA peritonitis generally resolves with antibiotic therapy and catheter retention. In contrast, MRSA infections are associated with higher rates of catheter removal, peritoneal membrane failure, and transition to hemodialysis.
Staphylococcus peritonitis remains a major challenge in peritoneal dialysis care. Its prompt recognition, early empiric antibiotic coverage, and tailored treatment based on microbiological data are essential to preventing long-term morbidity. Proactive infection control strategies, including decolonization and exit-site care, play a critical role in reducing incidence and recurrence. Optimal management of this condition requires collaboration between nephrology, infectious disease, and surgical teams to ensure successful outcomes.