Staphylococcus osteomyelitis is a serious bacterial infection of the bone caused primarily by Staphylococcus aureus. This pathogen can infiltrate bone tissue through hematogenous spread, direct inoculation from trauma or surgery, or contiguous spread from adjacent infections. The disease can present acutely or evolve into a chronic condition, leading to bone necrosis, abscess formation, and systemic complications if left untreated.
Etiology and Pathophysiology of Staphylococcal Bone Infections
Common Causative Organisms
- Staphylococcus aureus (MSSA and MRSA): Most frequent causative agent
- Coagulase-negative Staphylococci (e.g., S. epidermidis): Often associated with orthopedic implants
- Methicillin-resistant Staphylococcus aureus (MRSA): Leads to more severe and difficult-to-treat cases
Pathogenesis of Infection
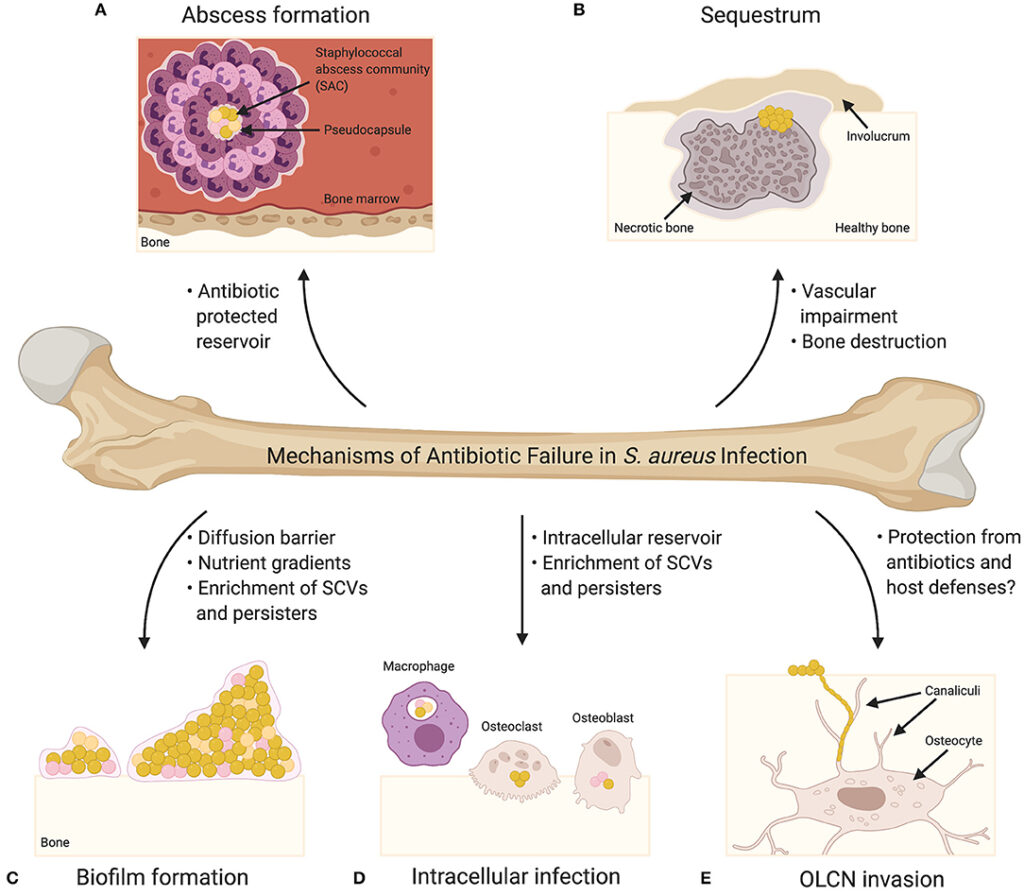
The pathogen invades bone tissue, adheres to osteoblasts, and secretes toxins and proteolytic enzymes, destroying bone matrix and forming sequestra. Biofilm formation on prosthetic material or necrotic bone further protects the bacteria from host defenses and antibiotics.
Risk Factors and Modes of Transmission
| Risk Factor | Description |
|---|---|
| Recent orthopedic surgery | Especially with implants or joint replacements |
| Open fractures or penetrating trauma | Direct exposure of bone to external contaminants |
| Diabetes mellitus | Impaired immunity and poor circulation |
| Intravenous drug use | Increases hematogenous seeding |
| Immunosuppression | Reduces host ability to contain infection |
| Hemodialysis or indwelling catheters | Serve as sources for bloodstream infection |
Clinical Presentation of Staphylococcal Osteomyelitis
Acute Osteomyelitis
- Rapid onset of pain and swelling
- Fever and systemic symptoms
- Erythema and warmth over affected area
- Restricted joint or limb movement
Chronic Osteomyelitis
- Persistent or intermittent pain
- Sinus tract formation with purulent discharge
- Localized swelling and deformity
- Low-grade fever or asymptomatic
Diagnostic Approach for Staphylococcus Osteomyelitis
Imaging Modalities
- X-ray: May show bone lysis and periosteal reaction after 10–14 days
- MRI: Most sensitive for early detection; identifies marrow edema and abscess
- CT Scan: Useful for detailed bone architecture and sequestrum visualization
- Radionuclide Bone Scans: Beneficial in multifocal or unclear cases
Microbiological and Laboratory Tests
- Blood cultures: Positive in hematogenous cases
- Bone biopsy and culture: Gold standard for pathogen identification
- ESR and CRP: Typically elevated in acute cases; useful for monitoring response
- WBC count: Often elevated but nonspecific
Classification of Osteomyelitis (Cierny-Mader System)
| Type | Description |
|---|---|
| Type I | Medullary (involving the marrow cavity) |
| Type II | Superficial (limited to cortical bone) |
| Type III | Localized full-thickness cortical involvement |
| Type IV | Diffuse (entire bone thickness with instability) |
Antimicrobial Treatment Strategies
Empirical Therapy
Initiated based on patient risk and local resistance patterns:
- Vancomycin (for suspected MRSA)
- Cefazolin or Nafcillin (for MSSA in stable patients)
- Linezolid or Daptomycin (MRSA with vancomycin intolerance)
Targeted Therapy
- Duration: Typically 4–6 weeks of IV therapy; can transition to oral step-down in some cases
- Oral agents: Clindamycin, Linezolid, TMP-SMX (based on susceptibility)
- Biofilm-active agents: Rifampin used in combination for prosthetic joint infections
Surgical Management and Interventions
Indications for Surgery
- Necrotic bone or abscess formation
- Failure of medical therapy
- Chronic osteomyelitis with sinus tract
- Implant-related infections
Surgical Procedures
- Debridement of infected and necrotic tissue
- Sequestrectomy and removal of prosthetic devices if needed
- Placement of antibiotic-impregnated beads or spacers
- Bone grafting or reconstruction in severe defects
Complications of Untreated or Inadequately Treated Infection
| Complication | Impact |
|---|---|
| Chronic osteomyelitis | Long-term disability and recurrence risk |
| Bone necrosis and structural loss | May require amputation or reconstruction |
| Septic arthritis | Especially in adjacent joints |
| Pathological fractures | Due to weakened bone architecture |
| Sepsis and systemic spread | Life-threatening in immunocompromised patients |
Prevention of Staphylococcal Osteomyelitis
Preoperative Measures
- Nasal decolonization of S. aureus carriers using mupirocin
- Perioperative antibiotic prophylaxis
- Strict aseptic surgical technique
Postoperative Care
- Monitoring for early signs of infection
- Proper wound care and drainage management
- Minimizing use of indwelling devices
Lifestyle and Chronic Disease Control
- Glycemic control in diabetic patients
- Avoidance of IV drug use
- Prompt treatment of superficial skin infections
Prognosis and Long-Term Outcomes
Prognosis depends on:
- Timeliness of diagnosis and intervention
- Pathogen involved (MRSA associated with worse outcomes)
- Host immune status
- Surgical accessibility for debridement
- Adherence to prolonged antibiotic therapy
With appropriate treatment, acute cases often resolve fully. Chronic cases may require long-term suppressive therapy or repeat interventions.
Staphylococcus osteomyelitis represents a challenging and potentially debilitating condition that necessitates a multidisciplinary approach involving prompt diagnosis, targeted antibiotic therapy, and surgical management when required. Prevention strategies and patient education remain crucial to minimizing recurrence and ensuring optimal recovery outcomes.

