Staphylococcus infections are caused by Staphylococcus bacteria, commonly found on the skin and in the nasal passages of healthy individuals. While typically harmless, certain strains can cause mild to severe infections when they invade the body through cuts, wounds, or medical devices. The most clinically significant species is Staphylococcus aureus, which includes methicillin-resistant strains (MRSA) that present serious public health challenges due to their antibiotic resistance.

Classification and Types of Staphylococcal Infections
1. Skin and Soft Tissue Infections (SSTIs)
- Boils (Furuncles): Painful, pus-filled bumps.
- Impetigo: Highly contagious superficial skin infection.
- Cellulitis: Rapidly spreading inflammation of skin and subcutaneous tissues.
- Abscesses: Localized collections of pus.
2. Respiratory Tract Infections
- Pneumonia due to S. aureus, particularly in ventilated or immunocompromised patients.
- Secondary bacterial pneumonia following influenza.
3. Bloodstream Infections
- Bacteremia: Presence of staphylococci in the bloodstream, potentially leading to sepsis.
- Septicemia: Severe systemic infection that may progress rapidly.
4. Bone and Joint Infections
- Osteomyelitis: Infection of the bone, often following trauma or surgery.
- Septic Arthritis: Infection within joints, usually requiring prompt drainage.
5. Device-Related Infections
- Prosthetic joint infections
- Infected vascular grafts
- Catheter-associated infections
6. Endocarditis
- Life-threatening infection of the inner lining of the heart, often affecting valves.
Causative Species and Pathogenesis
The most prominent staphylococcal pathogens include:
- Staphylococcus aureus: Coagulase-positive, frequently pathogenic.
- Staphylococcus epidermidis: Coagulase-negative, typically opportunistic in nature.
- Staphylococcus saprophyticus: Common cause of urinary tract infections in young women.
Virulence Factors
- Protein A: Inhibits opsonization and phagocytosis.
- Coagulase: Promotes clot formation, shielding bacteria.
- Toxins: Exfoliative toxins, enterotoxins, and toxic shock syndrome toxin (TSST-1).
- Biofilm production: Especially in device-related infections.
Transmission and Risk Factors
Staphylococcus spreads via direct contact, contaminated surfaces, or airborne droplets in healthcare settings.
Key Risk Factors:
- Open wounds or surgical incisions
- Indwelling medical devices
- Compromised immune systems
- Hospitalization or recent antibiotic use
- Close contact sports or shared personal items
Clinical Symptoms of Staphylococcus Infections
Symptoms vary with the type and severity of the infection:
| Type of Infection | Common Symptoms |
|---|---|
| Skin Infections | Redness, swelling, pus, warmth, pain |
| Pneumonia | Cough, chest pain, fever, breathing difficulty |
| Bacteremia | Fever, chills, low blood pressure, confusion |
| Bone Infections | Localized bone pain, swelling, fever |
| Endocarditis | Fatigue, heart murmur, petechiae, night sweats |
Diagnostic Approach
Laboratory Investigations
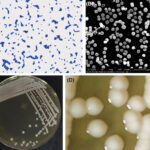
- Gram stain and culture of infected tissue or fluids.
- Blood cultures for suspected systemic involvement.
- Nucleic acid amplification tests (NAATs) for rapid detection.
- Antibiotic susceptibility testing to guide therapy.
Imaging
- X-rays, MRI, or CT scans for suspected bone, joint, or deep tissue involvement.
- Echocardiography for suspected endocarditis.
Antibiotic Therapy and Resistance Challenges
Methicillin-Sensitive Staphylococcus aureus (MSSA)
- First-line: Dicloxacillin, cefazolin, clindamycin
- Alternatives: Amoxicillin-clavulanate, cephalexin
Methicillin-Resistant Staphylococcus aureus (MRSA)
- Severe infections: Vancomycin, daptomycin, linezolid
- Mild to moderate infections: TMP-SMX, doxycycline, clindamycin
Resistance has complicated treatment regimens, making culture and sensitivity essential for effective therapy.
Preventive Strategies and Infection Control
Personal Hygiene
- Regular hand washing with soap or alcohol-based sanitizers.
- Avoid sharing personal items such as razors, towels, or athletic gear.
Wound Care
- Clean and cover all wounds promptly.
- Seek medical care for persistent or worsening lesions.
Hospital Protocols
- Contact precautions for infected patients.
- Sterilization of instruments and environmental cleaning.
- Surveillance cultures in high-risk settings (e.g., ICUs).
Complications and Long-Term Consequences
If untreated, staphylococcal infections can lead to:
- Chronic osteomyelitis
- Persistent abscess formation
- Septic shock
- Multiorgan failure
- Death in severe systemic cases
Prompt identification and targeted treatment reduce the risk of long-term damage or mortality.
Staphylococcus infections encompass a spectrum from minor skin conditions to life-threatening systemic diseases. With the rise of multidrug-resistant strains, clinical vigilance and evidence-based antibiotic use are essential. Prevention through hygiene, careful device management, and infection control protocols remains the cornerstone in reducing incidence and transmission.