Staphylococcus epidermidis, a coagulase-negative staphylococcus (CoNS), is primarily known as a benign skin commensal. However, in specific clinical settings, particularly involving urinary catheters and immunocompromised patients, it acts as an opportunistic uropathogen. Though often considered a contaminant in urine cultures, increasing cases highlight its role in true urinary tract infections (UTIs), especially nosocomial or device-related.
Microbiological Profile and Pathogenic Mechanisms
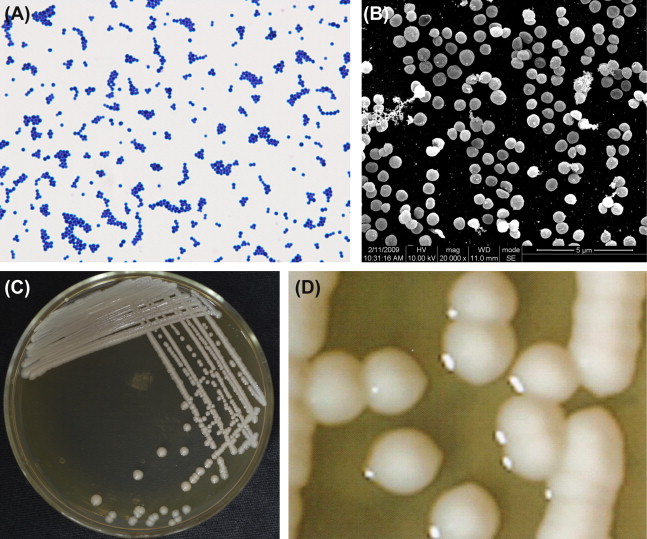
S. epidermidis is a Gram-positive, facultative anaerobe. It differs from S. aureus in its lack of aggressive toxins but compensates with key mechanisms:
- Biofilm formation: Protects from host defenses and antibiotics.
- Adherence to urinary catheters and epithelial surfaces: Enables colonization.
- Resistance genes (e.g., mecA): Confer methicillin resistance (MRSE), limiting therapeutic options.
These attributes allow S. epidermidis to persist in the urinary tract, especially under favorable conditions such as indwelling devices or altered immunity.
Risk Factors for Staphylococcus Epidermidis UTI
- Urinary catheters (Foley, suprapubic, intermittent)
- Neurogenic bladder or voiding dysfunction
- Elderly age
- Diabetes mellitus
- Hospitalization or long-term care facility stay
- Recent urologic procedures
- Immunosuppression (cancer, corticosteroids, transplant recipients)
Patients in these categories should be closely monitored for symptoms even if urine cultures reveal CoNS.
Clinical Presentation: Signs and Symptoms
The manifestation of S. epidermidis urinary tract infection may be subtle and often overlaps with catheter-associated asymptomatic bacteriuria. However, true infections typically present with:
- Dysuria (painful urination)
- Increased urinary frequency or urgency
- Suprapubic or flank pain
- Cloudy or foul-smelling urine
- Hematuria (blood in urine)
- Low-grade fever or malaise
- In catheterized patients: catheter blockage or leakage, sediment in tubing
Diagnostic Criteria and Laboratory Evaluation
Urine Culture Interpretation
S. epidermidis in urine cultures is often dismissed as a contaminant. However, the following support its clinical relevance:
- ≥10⁵ CFU/mL in clean-catch or catheter specimens
- Repeated isolation in symptomatic patients
- Pyuria or leukocyte esterase positivity in urinalysis
- Growth in anaerobic conditions or presence of biofilm
Supporting Tests
- Urinalysis: Leukocytes, nitrites, proteinuria
- Microscopy: White blood cells, bacteria, epithelial cells
- Blood cultures: If systemic symptoms are present
- Imaging (Ultrasound/CT KUB): In complicated cases or persistent infections
Pathogenesis in Catheter-Associated UTIs
Biofilms act as a nidus for infection, especially in long-term catheter use, making eradication difficult without device removal.
Antibiotic Therapy for S. epidermidis UTI
Empiric Regimen
Empiric therapy should be guided by clinical severity and the likelihood of methicillin resistance.
- Vancomycin: Primary IV option for suspected MRSE
- Linezolid: Suitable oral alternative, especially in outpatient settings
- Trimethoprim-sulfamethoxazole (TMP-SMX): Considered if susceptibility confirmed
- Nitrofurantoin or Fosfomycin: For lower tract infections in catheter-free patients with susceptible isolates
Targeted Therapy
Antibiotic choice must be refined once culture and susceptibility results are available. Therapy duration typically ranges from 7 to 14 days, extended in complicated or relapsing infections.
Device Management and Supportive Care
- Catheter replacement: Mandatory in confirmed infection
- Temporary catheter removal: Facilitates eradication of biofilm-associated bacteria
- Hydration and bladder irrigation: May assist in mechanical flushing of bacteria
- Urinary acidification: Limits bacterial growth (e.g., ascorbic acid supplementation)
Complications of Untreated or Recurrent Infection
- Pyelonephritis
- Urosepsis
- Prostatitis
- Bladder or renal abscess
- Chronic bacteriuria
- Recurrent urinary tract infections
Recurrent S. epidermidis UTIs necessitate urologic evaluation for anatomical or functional abnormalities.
Differentiating Contamination from True Infection
It is essential to distinguish incidental contamination from pathogenic infection. Use the following decision matrix:
This helps avoid overtreatment while ensuring infections are not missed in high-risk patients.
Prevention Strategies in Healthcare Settings
- Strict catheter hygiene protocols
- Avoidance of unnecessary catheterization
- Prompt removal of catheters when no longer indicated
- Closed drainage systems
- Staff training on aseptic techniques
- Patient education on symptoms of UTI
These interventions significantly reduce the incidence of catheter-associated S. epidermidis urinary infections.
Staphylococcus epidermidis, though traditionally regarded as a benign contaminant, has emerged as a notable cause of urinary tract infections in select populations. Accurate diagnosis, supported by clinical and microbiological evidence, is essential for appropriate management. By integrating targeted antimicrobial therapy, vigilant device management, and preventative strategies, healthcare providers can effectively manage and reduce the burden of S. epidermidis UTIs.

