Staphylococcus endometritis is an inflammatory infection of the endometrial lining of the uterus caused by Staphylococcus species, most commonly Staphylococcus aureus and Staphylococcus epidermidis. Though less frequent than polymicrobial or gram-negative infections, Staphylococcus-induced endometritis remains clinically significant due to its potential for systemic dissemination, especially in postpartum or post-surgical settings.
Epidemiology and Risk Factors
Staphylococcal endometritis is more likely to occur in specific high-risk populations:
- Postpartum women, particularly following cesarean delivery
- Post-abortion cases, especially after non-sterile procedures
- Patients with intrauterine devices (IUDs)
- Recent uterine instrumentation or surgery
- Immunocompromised individuals
- Hospitalized patients exposed to nosocomial Staphylococcus strains
Staphylococcus aureus (both MSSA and MRSA) is commonly implicated in acute presentations, while coagulase-negative staphylococci may cause subacute or chronic inflammation.
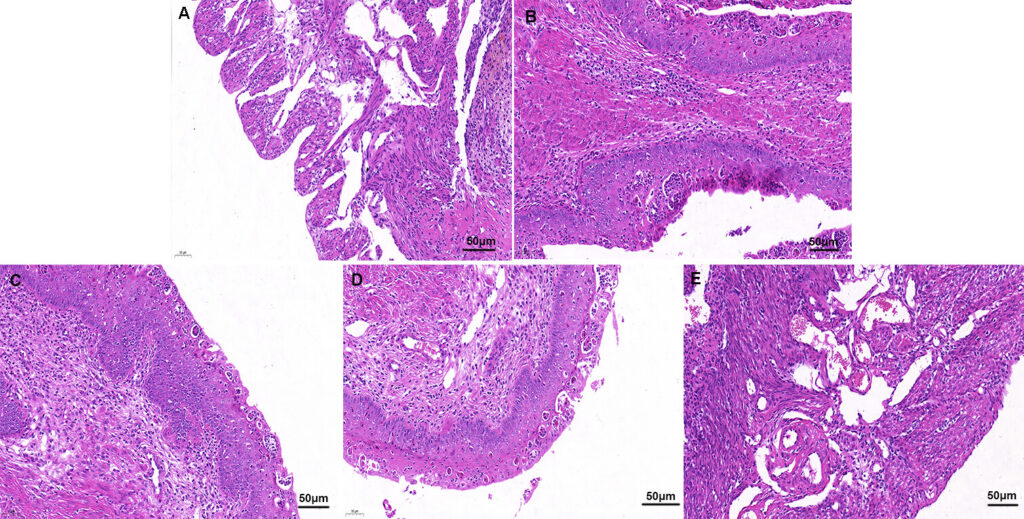
Pathophysiology of Staphylococcus-Induced Endometritis
Staphylococci gain access to the uterine cavity either by ascending migration through the cervix or via hematogenous spread. They adhere to endometrial tissue, evading immune detection with biofilm formation (notably S. epidermidis) and secreting virulence factors that incite inflammation.
Clinical Manifestations
The symptomatology of staphylococcal endometritis may vary depending on the severity and acuteness of the infection:
- Fever (often >38.5°C)
- Lower abdominal or pelvic pain
- Foul-smelling lochia (in postpartum patients)
- Uterine tenderness
- Abnormal uterine bleeding
- Leukocytosis
- Chills and malaise
In severe cases, signs of systemic involvement such as hypotension or tachycardia may indicate progression to sepsis.
Diagnostic Evaluation
Pelvic Examination
- Assess for cervical motion tenderness
- Evaluate for uterine enlargement or tenderness
Laboratory Testing
- Complete blood count (CBC): Elevated white blood cell count
- CRP and ESR: Markers of systemic inflammation
- Endometrial culture: Gold standard for pathogen identification
- Blood cultures: Necessary if bacteremia is suspected, particularly with S. aureus
Imaging
- Pelvic ultrasound: May show retained products of conception, intrauterine fluid, or abscess formation
- MRI or CT scan: Useful in complicated or unresponsive cases to rule out pelvic abscess or pyometra
Common Causative Staphylococcal Species
| Species | Characteristics | Clinical Relevance |
|---|---|---|
| S. aureus (MSSA/MRSA) | Coagulase-positive, virulent | Common in postpartum and post-surgical infections |
| S. epidermidis | Coagulase-negative, biofilm-forming | Associated with IUD-related or chronic endometritis |
| S. saprophyticus | Uropathogen | Rarely causes endometritis, more common in urinary infections |
Antimicrobial Management of Staphylococcus Endometritis
Empiric Therapy
Initiation of broad-spectrum antibiotics is critical pending culture results. Regimens should include MRSA coverage in high-risk patients.
Recommended Regimens:
- IV Clindamycin + Gentamicin (standard postpartum coverage)
- Add Vancomycin if MRSA is suspected or confirmed
- Alternative for Penicillin Allergy: Linezolid or Daptomycin (based on susceptibility)
Duration:
- 7–14 days, depending on clinical response
- May transition to oral antibiotics upon defervescence and clinical improvement
Surgical and Supportive Management
- Evacuation of retained products of conception in cases of incomplete abortion
- Removal of intrauterine devices in IUD-associated infections
- Drainage of abscesses if identified via imaging
- Supportive care: Antipyretics, IV fluids, and monitoring for sepsis
Complications of Untreated or Refractory Infection
- Pelvic abscess formation
- Pyometra
- Infertility due to scarring and adhesions (Asherman’s syndrome)
- Chronic pelvic pain
- Bacteremia and sepsis
- Endocarditis (especially with S. aureus)
Prevention Strategies
- Strict aseptic techniques during gynecologic procedures
- Proper sterilization of surgical instruments
- Screening and decolonization for MRSA in high-risk patients
- Prophylactic antibiotics for cesarean section and D&C procedures
- Avoidance of unnecessary uterine instrumentation
Prognosis
When promptly diagnosed and treated, the prognosis for staphylococcal endometritis is favorable. However, delays in therapy or incomplete treatment can result in significant morbidity, including infertility and systemic complications. Persistent symptoms warrant further investigation for retained tissue, abscess, or resistant organisms.
Staphylococcus endometritis, though less common than polymicrobial causes, requires heightened clinical suspicion, particularly in postpartum and post-procedural settings. Early initiation of appropriate antibiotics, source control, and close monitoring are critical for favorable outcomes. Understanding the microbial landscape and resistance patterns is essential to ensure effective management and reduce recurrence.