Atrial fibrillation (AFib) is a common cardiac arrhythmia characterized by irregular and often rapid heart rhythms. Cardioversion, a standard treatment for AFib, aims to restore a normal sinus rhythm. This article provides an in-depth understanding of the cardioversion procedure, its types, indications, risks, and what patients can expect before and after treatment.
Understanding Cardioversion
Cardioversion is a medical intervention designed to correct abnormal heart rhythms. It can be performed using electrical or pharmacological methods. Both aim to synchronize the heart’s electrical activity and restore normal rhythm, but their application depends on the patient’s specific medical condition.
Types of Cardioversion
- Electrical Cardioversion
- Involves delivering controlled electric shocks to the heart through electrodes placed on the chest.
- Typically performed under sedation to minimize discomfort.
- Often used when rapid restoration of normal rhythm is required.
- Pharmacological Cardioversion
- Involves administering antiarrhythmic drugs to stabilize the heart’s rhythm.
- Suitable for patients where electrical cardioversion is not preferred or contraindicated.
- Common medications include amiodarone, flecainide, and propafenone.
Indications for Cardioversion
Cardioversion is typically recommended in cases where:
- AFib causes significant symptoms like palpitations, fatigue, or shortness of breath.
- There is a high risk of stroke due to ineffective blood flow in the atria.
- The arrhythmia is new-onset or paroxysmal and amenable to rhythm restoration.
Preparation for Cardioversion
Diagnostic Workup
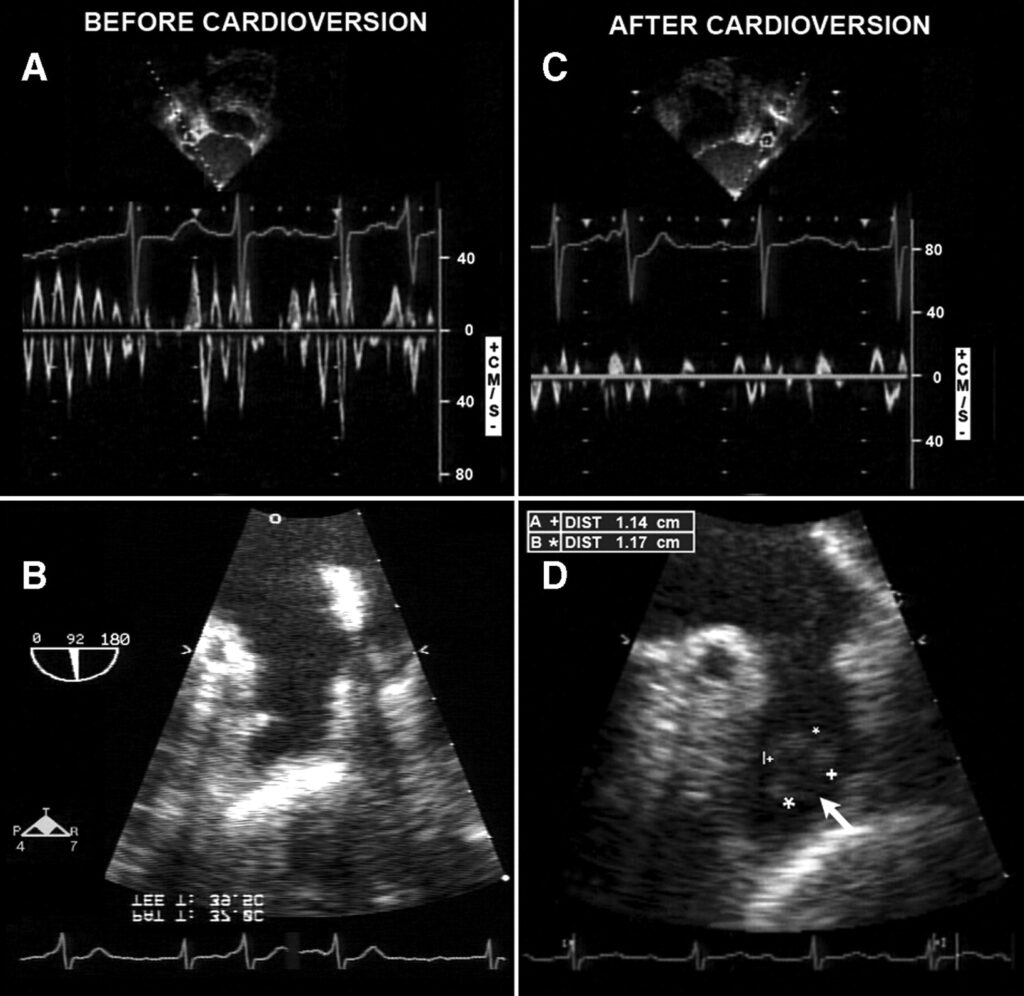
- Electrocardiogram (ECG): Confirms the presence of AFib.
- Echocardiogram: Identifies structural heart issues and evaluates the presence of blood clots.
- Blood Tests: Assesses overall health and ensures safe drug administration.
Anticoagulation Therapy
To minimize stroke risk, patients may require anticoagulants like warfarin or direct oral anticoagulants (DOACs) for 3-4 weeks before and after cardioversion.
The Cardioversion Procedure
Electrical Cardioversion
- Preparation
- Patient is sedated and monitored.
- Pads or paddles are positioned on the chest and back.
- Delivery of Shock
- A synchronized shock is delivered to reset the heart’s electrical activity.
- Post-Procedure Monitoring
- Heart rhythm and vital signs are closely observed for complications.
Pharmacological Cardioversion
- Drug Administration
- Antiarrhythmic drugs are administered orally or intravenously.
- Monitoring
- Continuous ECG monitoring ensures effectiveness and detects adverse reactions.
Risks and Complications
Although cardioversion is generally safe, potential risks include:
- Stroke: Due to dislodged blood clots.
- Arrhythmias: New or worsening irregular heart rhythms.
- Burns or Irritation: From electrode pads during electrical cardioversion.
- Medication Side Effects: Including dizziness, low blood pressure, or allergic reactions.
Recovery and Follow-Up
Post-Procedure Care
- Most patients can resume normal activities within a day.
- Adherence to prescribed anticoagulants is critical to prevent stroke.
- Lifestyle changes, such as reducing alcohol and caffeine intake, may improve long-term outcomes.
Long-Term Monitoring
- Regular follow-ups with a cardiologist ensure rhythm stability.
- Additional interventions, such as ablation, may be considered for recurrent AFib.
MYHEALTHMAG