Chronic bronchitis, defined by persistent inflammation of the bronchial tubes with productive cough for at least three months in two consecutive years, is a subtype of chronic obstructive pulmonary disease (COPD). While viral and gram-negative bacterial infections are more commonly implicated in exacerbations, Staphylococcus aureus—particularly methicillin-resistant strains (MRSA)—is an emerging concern in both acute exacerbations and persistent colonization of the bronchial mucosa.
Pathophysiology of Staphylococcus-Associated Chronic Bronchitis
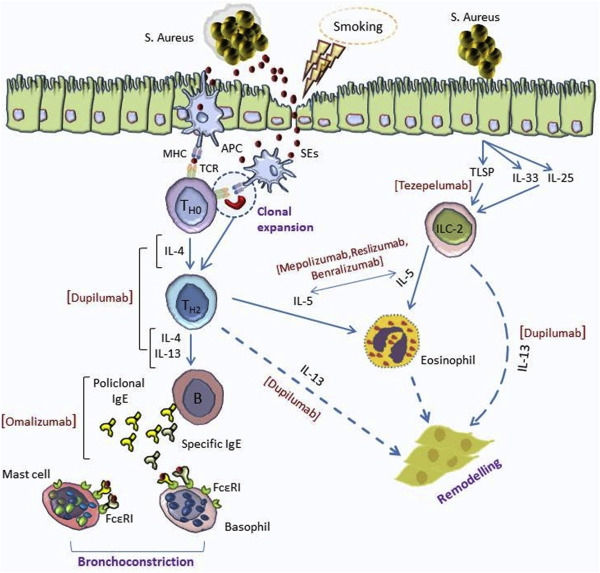
Staphylococcus aureus can either colonize the lower respiratory tract or act as a pathogen in the setting of mucosal damage and impaired mucociliary clearance.
- Biofilm Formation: Allows S. aureus to persist on damaged mucosa, evading host defenses and antibiotics.
- Toxin Production: Exfoliative toxins and leukocidins contribute to mucosal injury.
- Superinfection: Often follows viral respiratory infections or other bacterial colonization.
Risk Factors for Staphylococcal Chronic Bronchitis
- Advanced COPD (GOLD stage III–IV)
- Frequent hospitalizations or ICU admissions
- Long-term corticosteroid therapy
- Use of broad-spectrum antibiotics
- Prior colonization with MRSA
- Tracheostomy or prolonged mechanical ventilation
- Structural lung disease (e.g., bronchiectasis)
Clinical Features of Staphylococcus-Induced Exacerbations
Patients with staphylococcal involvement in chronic bronchitis often present with:
- Increased cough frequency and sputum volume
- Purulent, often yellow-green sputum
- Dyspnea and wheezing
- Low-grade fever
- Malaise and fatigue
- Pleuritic chest pain (in more severe cases)
Exacerbations may be more frequent and prolonged, especially in MRSA-colonized individuals.
Diagnostic Approach to Staphylococcal Chronic Bronchitis
Sputum Analysis and Culture
- Gram stain: Gram-positive cocci in clusters
- Culture: Essential to differentiate MSSA from MRSA
- Quantitative culture: Helps determine colonization vs infection threshold
Molecular Diagnostics
- PCR assays to rapidly detect MRSA
- 16S rRNA sequencing in complex cases with polymicrobial flora
Imaging Studies
- Chest X-ray: May show increased bronchovascular markings
- High-Resolution CT (HRCT): Evaluates for bronchiectasis or post-infectious scarring
Inflammatory Markers
- Elevated C-reactive protein (CRP) and procalcitonin may suggest bacterial exacerbation
Management of Staphylococcus-Associated Chronic Bronchitis
Antibiotic Therapy
Empirical Treatment
Initiated based on clinical severity, pending culture results.
| Suspected Pathogen | Oral Options | IV Options | Duration |
|---|---|---|---|
| MSSA | Amoxicillin-clavulanate, Doxycycline | Cefazolin, Nafcillin | 7–10 days |
| MRSA | Clindamycin, Linezolid, TMP-SMX | Vancomycin, Linezolid, Daptomycin | 10–14 days (or longer in recurrent cases) |
Note: Fluoroquinolones are generally avoided due to rising resistance rates and QT prolongation risks.
Airway Clearance and Adjunct Therapies
- Nebulized bronchodilators (e.g., albuterol)
- Inhaled corticosteroids to reduce bronchial inflammation
- Mucolytic agents (e.g., N-acetylcysteine)
- Pulmonary rehabilitation in chronic cases
MRSA Decolonization (for recurrent infections)
- Nasal mupirocin
- Chlorhexidine body washes
- Rifampin + doxycycline in select persistent carriers (with ID consultation)
Chronic Colonization vs Active Infection
It is vital to distinguish between colonization and active infection, particularly in sputum cultures from COPD patients.
| Feature | Colonization | Infection |
|---|---|---|
| Sputum volume | Stable | Increased |
| Sputum appearance | Clear/mucoid | Purulent or blood-tinged |
| Systemic symptoms | Absent | Present (fever, malaise) |
| Inflammatory markers | Normal | Elevated |
| Imaging changes | Stable | New infiltrates |
Prevention of Staphylococcal Exacerbations
Vaccination and General Measures
- Annual influenza vaccine
- Pneumococcal vaccination
- Smoking cessation
- Avoidance of unnecessary antibiotics
Infection Control
- Rigorous hand hygiene
- Contact precautions for MRSA-positive patients
- Environmental decontamination in healthcare settings
Long-Term Macrolide Therapy
In select COPD patients with frequent exacerbations, low-dose azithromycin may reduce frequency—but increases risk of resistance.
Prognosis and Long-Term Outcomes
The presence of Staphylococcus aureus, especially MRSA, in chronic bronchitis is associated with:
- Increased hospital readmissions
- Prolonged exacerbation duration
- Declining pulmonary function
- Higher mortality in advanced COPD
Close follow-up, pulmonary function monitoring, and timely antimicrobial therapy are critical to improving quality of life and outcomes.
Staphylococcus aureus plays a significant role in chronic bronchitis, especially among individuals with advanced pulmonary disease and frequent healthcare exposure. Its ability to persist in the airway through biofilm formation and evade host defenses underscores the need for precise microbiological diagnosis and tailored antimicrobial therapy. Effective management hinges on a multidisciplinary approach, encompassing pharmacologic intervention, airway hygiene, preventive strategies, and patient education.