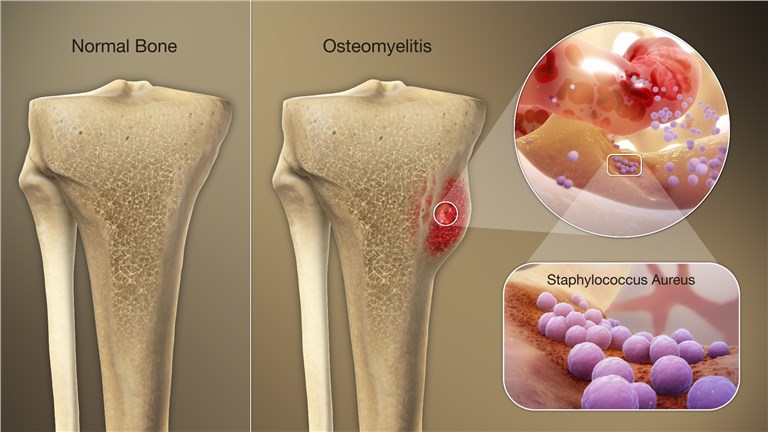
Staphylococcus aureus is the most prevalent pathogen causing osteomyelitis, an infection of the bone characterized by inflammation, necrosis, and new bone formation. This organism exhibits a high affinity for bone tissue, facilitated by surface adhesins, biofilm formation, and immune evasion mechanisms. Both methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) strains pose significant clinical challenges due to persistent infection and recurrence risk.
Pathophysiology of S. aureus Osteomyelitis
Osteomyelitis occurs when S. aureus gains access to bone tissue through hematogenous spread, direct inoculation (surgical or traumatic), or contiguous soft tissue infection. Once present, the bacteria adhere to the bone matrix and osteoblasts, initiating an inflammatory response and forming protective biofilms that hinder immune clearance and antibiotic penetration.
Classification of Osteomyelitis by Infection Source
- Hematogenous Osteomyelitis
- Common in children and elderly
- Typically affects long bones or vertebrae
- Caused by bloodstream spread
- Contiguous Osteomyelitis
- Result of spread from adjacent tissue infections or ulcers
- Frequent in patients with diabetes or pressure sores
- Post-Traumatic/Post-Surgical Osteomyelitis
- Following open fractures, implants, or orthopedic procedures
- Biofilm formation on hardware complicates management
- Chronic Osteomyelitis
- Persistent infection with necrotic bone (sequestrum)
- Often requires surgical debridement
Risk Factors for Staphylococcal Bone Infection
- Diabetes mellitus and peripheral vascular disease
- Immunosuppression
- Recent orthopedic surgery or fracture
- Presence of prosthetic material
- Intravenous drug use
- Chronic ulcers or pressure wounds
- Pediatric age (hematogenous spread more common)
Clinical Features of S. aureus Osteomyelitis
Acute Osteomyelitis
- Localized bone pain and tenderness
- Erythema, swelling, and warmth
- Fever and systemic symptoms
- Limited mobility in affected limb or joint
Chronic Osteomyelitis
- Persistent or intermittent drainage
- Sinus tract formation
- Reduced inflammatory signs
- History of previous infection or surgery
Diagnostic Evaluation of Osteomyelitis
Laboratory Tests
- Elevated ESR and CRP (sensitive but non-specific)
- Leukocytosis in acute cases
- Blood cultures positive in 50–70% of hematogenous osteomyelitis
Imaging Studies
- X-ray: May show bone lysis or periosteal elevation (delayed)
- MRI: Gold standard for early diagnosis, shows marrow edema and abscess
- CT scan: Useful for cortical bone and sequestrum detection
- Bone scan: Alternative in patients with MRI contraindications
Microbiological Confirmation
- Bone biopsy and culture (mandatory in chronic or refractory cases)
- Aspiration of abscess or joint fluid when accessible
- Identification of MSSA or MRSA crucial for targeted therapy
Antibiotic Treatment Strategies for S. aureus Osteomyelitis
Empiric Therapy
- Initiated before culture results in acutely ill patients
- Coverage for both MSSA and MRSA recommended:
- Vancomycin (MRSA)
- Cefazolin or nafcillin (MSSA)
Definitive Therapy
- Tailored based on susceptibility:
- MSSA: Nafcillin, oxacillin, cefazolin
- MRSA: Vancomycin, daptomycin, linezolid
- Duration: Typically 4–6 weeks IV; oral step-down may follow
- Suppressive therapy in non-surgical cases with retained hardware
Surgical Management of Osteomyelitis
Surgical intervention is often necessary in chronic or non-responsive infections:
- Debridement: Removal of necrotic tissue and sequestra
- Abscess drainage
- Hardware removal (if biofilm is present and device is non-essential)
- Reconstruction with bone grafting or vascularized flaps
- Amputation in severe, limb-threatening cases
Pediatric Considerations in Osteomyelitis
- Hematogenous spread is more common
- Long bones frequently involved
- Prompt antibiotic therapy typically effective
- Surgical drainage reserved for abscess or joint involvement
Complications of Untreated or Recurrent S. aureus Osteomyelitis
- Chronic infection with sinus tract formation
- Pathological fractures
- Growth disturbances in children
- Sepsis and systemic spread
- Amputation in severe diabetic foot infections
Preventive Measures Against Osteomyelitis
In Hospital Settings
- Proper surgical site sterilization
- Prophylactic antibiotics for orthopedic procedures
- Screening and decolonization for S. aureus nasal carriers
In Community and Chronic Care Settings
- Foot care in diabetics to prevent ulcers
- Prompt treatment of skin infections
- Avoidance of unnecessary invasive procedures
- Patient education on wound hygiene
Prognosis and Long-Term Management
Prognosis depends on early detection, pathogen resistance profile, adequacy of debridement, and comorbid conditions.
Better Outcomes in:
- Early-diagnosed MSSA infections
- Pediatric patients
- Surgically treated cases with complete debridement
Poor Prognosis associated with:
- MRSA infection
- Delayed treatment
- Comorbidities like diabetes, PVD
- Retained infected hardware
Staphylococcus aureus osteomyelitis demands a prompt and aggressive approach to prevent lasting skeletal damage and systemic complications. Accurate microbiological diagnosis, prolonged antibiotic therapy, and thorough surgical management form the cornerstone of effective treatment. Continued vigilance in high-risk populations and adherence to preventive protocols can significantly reduce disease burden and improve clinical outcomes.

