Staphylococcus aureus is the leading bacterial cause of joint infections, frequently resulting in septic arthritis and prosthetic joint infections (PJI). Its ability to adhere to synovial membranes and form biofilms makes it particularly dangerous. Prompt diagnosis and effective intervention are essential to prevent joint destruction, systemic spread, and long-term disability.
Pathogenesis of Staphylococcal Joint Infection
Joint infection typically begins with hematogenous spread of S. aureus from a distant source, although direct inoculation during surgery or trauma is also common. Once inside the joint, the organism rapidly proliferates in synovial fluid, triggering a severe inflammatory cascade.
Risk Factors for Staphylococcus aureus Joint Infections
Several patient-related and iatrogenic factors increase susceptibility:
- Advanced age
- Diabetes mellitus
- Rheumatoid arthritis
- Immunosuppression (e.g., chemotherapy, HIV)
- Joint prostheses or recent orthopedic surgery
- Intravenous drug use
- Pre-existing skin or soft tissue infections
- Hemodialysis or invasive vascular access
Clinical Presentation of Staphylococcal Joint Infections
The hallmark features of S. aureus joint infections include:
- Acute onset monoarthritis, commonly in the knee, hip, shoulder, or ankle
- Severe joint pain, swelling, erythema, and warmth
- Decreased range of motion
- Fever and systemic signs of infection
- In prosthetic joints: persistent pain, loosening, and joint effusion
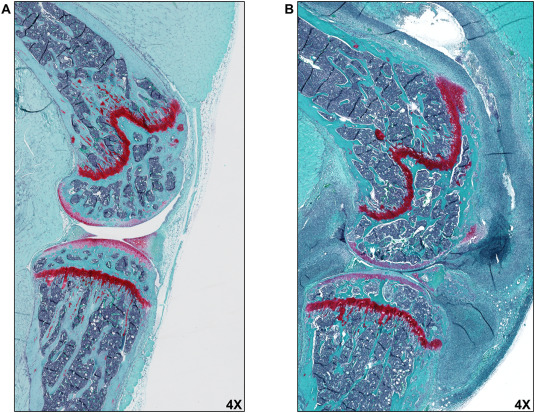
Without treatment, the infection rapidly erodes articular cartilage and may cause irreversible joint destruction within days.
Diagnostic Approach to S. aureus Septic Arthritis
Synovial Fluid Analysis
The most definitive diagnostic step involves aspiration of synovial fluid, followed by:
- Gram stain and culture: Gram-positive cocci in clusters
- Leukocyte count: Often >50,000/mm³ with >90% neutrophils
- Crystals: To rule out gout or pseudogout
- PCR or NAAT: Rapid identification of S. aureus DNA in certain cases
Blood Cultures
At least two sets should be drawn; positive cultures support the diagnosis and aid in identifying hematogenous origin.
Imaging
- X-ray: May reveal soft tissue swelling, joint space narrowing in chronic cases
- Ultrasound: Useful for effusion detection and guided aspiration
- MRI: Sensitive for early detection of joint and adjacent bone involvement
Distinction Between MSSA and MRSA Joint Infections
Methicillin-susceptible S. aureus (MSSA) infections typically respond well to beta-lactam antibiotics. In contrast, methicillin-resistant S. aureus (MRSA) requires alternative agents and carries a worse prognosis.
Clinical Considerations:
- MRSA: More common in healthcare-associated and post-surgical infections
- MSSA: Predominant in community-acquired septic arthritis
Treatment of Staphylococcus aureus Joint Infections
Antibiotic Therapy
Initiation of empiric intravenous antibiotics should not be delayed in suspected septic arthritis, especially in febrile or hemodynamically unstable patients.
Empiric Options:
- Vancomycin for MRSA coverage
- Ceftriaxone or cefazolin for MSSA if MRSA risk is low
Targeted Therapy:
- MSSA: Nafcillin, oxacillin, or cefazolin
- MRSA: Vancomycin or daptomycin
- Duration: Typically 4–6 weeks, based on clinical response and imaging
Surgical Management
Drainage of purulent material is critical. Options include:
- Needle aspiration: For superficial or small effusions
- Arthroscopic washout: Minimally invasive, highly effective
- Open arthrotomy: Required for deep or complex infections
Prosthetic Joint Infection (PJI)
Management strategies depend on timing and severity:
- DAIR (Debridement, Antibiotics, Implant Retention): For early-onset infections
- One- or two-stage revision arthroplasty: For chronic infections
- Long-term suppressive antibiotics: In patients unfit for surgery
Complications of Untreated or Refractory Infections
Failure to control S. aureus joint infection can result in:
- Joint ankylosis and permanent disability
- Osteomyelitis
- Sepsis and multiorgan failure
- Prosthetic joint failure
- Bacteremia and metastatic infections
Prognosis and Outcomes
Outcomes depend heavily on early diagnosis and the pathogen’s resistance profile. Timely surgical and antibiotic management yields favorable results in most patients.
Prognostic Factors:
- Advanced age
- MRSA vs MSSA (MRSA linked to higher morbidity)
- Delay in drainage or inadequate antibiotic therapy
- Immunocompromised status
Mortality Rates:
- General septic arthritis: ~10%
- MRSA infections: Up to 25%, especially in older adults
Prevention of Staphylococcal Joint Infections
In Surgical Settings
- Preoperative decolonization for S. aureus carriers (e.g., nasal mupirocin, chlorhexidine washes)
- Perioperative antibiotic prophylaxis
- Strict aseptic technique in orthopedic surgeries
In Community Settings
- Prompt treatment of skin infections
- Avoidance of intra-articular injections in infected individuals
- Early recognition and management of bloodstream infections
Staphylococcus aureus joint infections represent a serious clinical emergency requiring rapid intervention. Early joint aspiration, pathogen-specific antibiotic therapy, and timely surgical drainage are crucial in reducing joint damage and systemic spread. Understanding risk factors, diagnostic protocols, and treatment guidelines is essential to improving outcomes in both native and prosthetic joint infections.