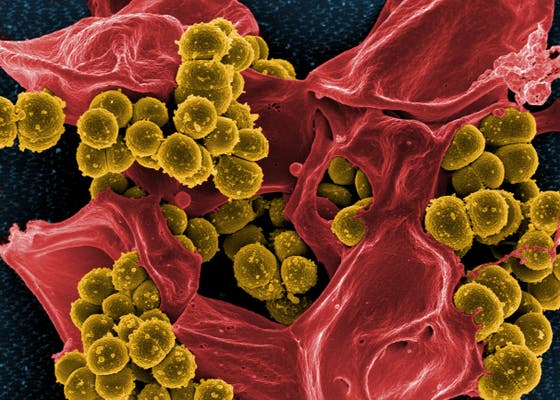
Staphylococcus aureus is one of the most virulent and common causative agents of infective endocarditis (IE), especially in both community-acquired and healthcare-associated settings. Its aggressive tissue invasion and high capacity for bloodstream persistence result in rapid valvular destruction, embolic events, and metastatic infections. S. aureus endocarditis affects both native and prosthetic valves and requires immediate medical attention due to its high morbidity and mortality.
Pathophysiology of Staphylococcal Endocarditis
The development of S. aureus endocarditis begins with bacterial adhesion to damaged or inflamed endocardial surfaces, often valves. Once attached, the organism forms biofilms and activates coagulation pathways, promoting the formation of vegetations—masses of platelets, fibrin, microorganisms, and inflammatory cells.
Risk Factors for S. aureus Infective Endocarditis
Patients at increased risk for S. aureus IE typically present with underlying medical conditions or exposure to healthcare environments:
- Intravenous drug use (IVDU)
- Prosthetic heart valves or intracardiac devices
- Congenital or rheumatic heart disease
- Hemodialysis or central venous catheters
- Recent cardiac surgery
- Immunosuppression (transplant recipients, chemotherapy)
Clinical Manifestations of S. aureus Endocarditis
The presentation of S. aureus endocarditis varies based on the affected valve and host immune status. Common symptoms include:
- High-grade, persistent fever
- Chills and rigors
- New or changing heart murmur
- Malaise and fatigue
- Signs of systemic emboli (stroke, organ infarction, Janeway lesions)
- Petechiae, splinter hemorrhages, and Osler nodes
- Septic pulmonary emboli (right-sided endocarditis)
- Congestive heart failure (left-sided endocarditis)
Right-sided endocarditis, common in IVDU, often presents with septic pulmonary emboli. Left-sided endocarditis is more severe and often leads to systemic embolism and valve destruction.
Diagnostic Approach to Staphylococcus aureus Endocarditis
Modified Duke Criteria
Diagnosis is based on clinical, microbiological, and echocardiographic findings. The Modified Duke Criteria remains the gold standard.
Blood Cultures
- Obtain at least three sets of blood cultures from different venipuncture sites prior to antibiotic administration.
- Persistent S. aureus bacteremia strongly suggests endocarditis.
Echocardiography
- Transesophageal echocardiogram (TEE) is preferred due to superior sensitivity in detecting vegetations, abscesses, or prosthetic valve involvement.
- Transthoracic echocardiogram (TTE) is an initial step, especially in low-risk patients.
Laboratory Investigations
- Elevated ESR and CRP
- Leukocytosis
- Hematuria and proteinuria (due to glomerulonephritis)
- Positive rheumatoid factor in subacute cases
Distinction Between MRSA and MSSA Endocarditis
Methicillin-resistant Staphylococcus aureus (MRSA) causes more aggressive disease with limited antibiotic options and higher mortality. Patients with healthcare exposure, indwelling devices, or prior antibiotic use are particularly vulnerable.
Methicillin-susceptible S. aureus (MSSA) endocarditis typically responds better to conventional beta-lactam antibiotics but still requires prolonged and intensive therapy.
Treatment Strategies for S. aureus Endocarditis
Empiric Antibiotic Therapy
Initiate empiric coverage in critically ill patients suspected of S. aureus IE until culture results guide definitive therapy.
Empiric regimen:
- Vancomycin ± cefepime (for MRSA and Gram-negative coverage)
Definitive Therapy Based on Susceptibility
For MSSA:
- Nafcillin or oxacillin (IV, 6 weeks)
- Cefazolin as an alternative for non-anaphylactic penicillin allergy
For MRSA:
- Vancomycin (IV, trough levels 15–20 µg/mL)
- Daptomycin (high-dose, ≥8 mg/kg/day)
Combination therapy with rifampin and gentamicin may be considered for prosthetic valve endocarditis but requires caution due to toxicity.
Duration of Therapy
- Native valve endocarditis: 4–6 weeks
- Prosthetic valve endocarditis: Minimum of 6 weeks
- Shorter durations are inadequate due to deep-seated biofilms and slow bacterial eradication
Indications for Surgical Intervention
Early surgical consultation is essential in the presence of:
- Heart failure due to valvular dysfunction
- Large vegetations (>10 mm) with embolic events
- Persistent bacteremia >5–7 days
- Perivalvular abscess or fistula formation
- Prosthetic valve dehiscence or obstruction
- Fungal or highly resistant infections
Complications of Untreated or Delayed Treatment
Failure to promptly diagnose and treat S. aureus endocarditis can result in:
- Valve perforation or rupture
- Embolic stroke or infarction (brain, spleen, kidneys)
- Septic shock
- Mycotic aneurysms
- Metastatic infections: vertebral osteomyelitis, septic arthritis
- High mortality (>30% in MRSA)
Prognosis and Mortality Trends
The prognosis of S. aureus endocarditis is significantly worse than other bacterial etiologies due to:
- Rapid progression
- High embolic potential
- Resistance patterns (MRSA)
- Comorbid conditions
Mortality Rates:
- MSSA IE: ~20–25%
- MRSA IE: ~30–40%
- Prosthetic valve infections: Higher mortality due to surgical complexity
Early diagnosis, appropriate antibiotics, and timely surgery improve outcomes.
Prevention and Infection Control
Hospital Settings
- MRSA screening and decolonization protocols
- Strict aseptic technique during catheter and device insertion
- Early removal of unnecessary intravascular lines
- Antibiotic prophylaxis before invasive procedures in high-risk individuals
Intravenous Drug Use
- Harm reduction programs
- Access to clean needles
- Education on endocarditis symptoms and early medical care
Staphylococcus aureus endocarditis remains one of the most aggressive and lethal forms of infective endocarditis. Prompt identification through blood cultures and echocardiography, combined with pathogen-specific antibiotic therapy and timely surgical intervention, is critical. In light of increasing MRSA prevalence, infection prevention, risk factor management, and patient education are key components in reducing incidence and improving patient outcomes.