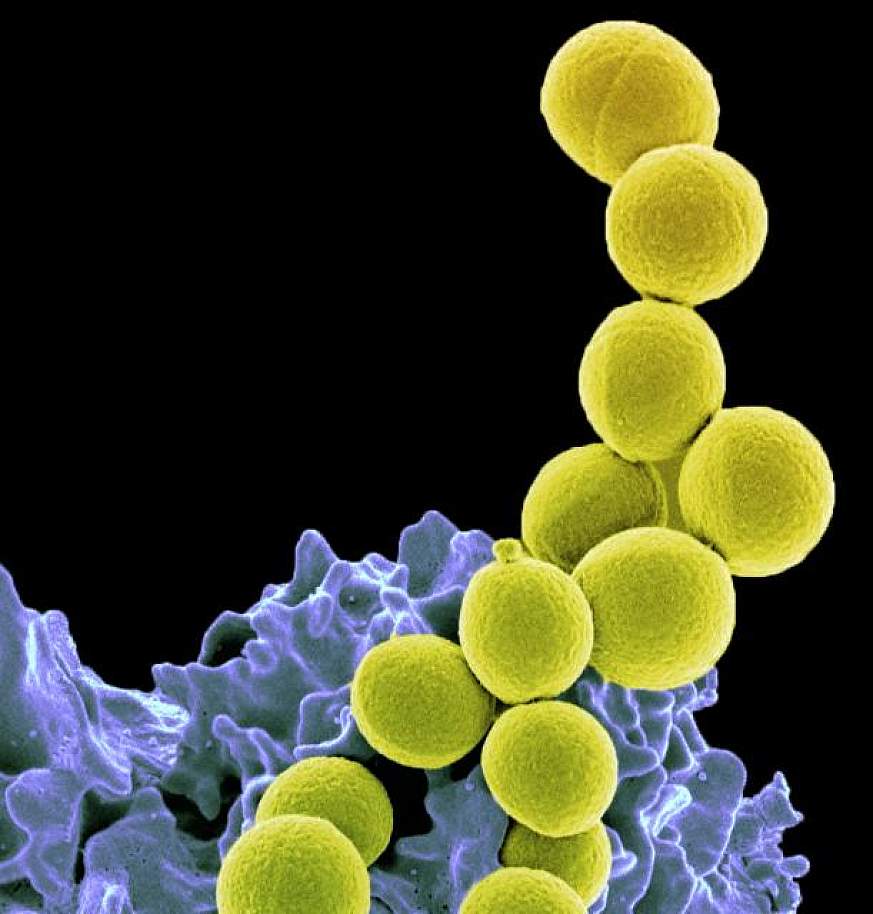
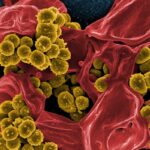
Staphylococcus aureus, a gram-positive coccal bacterium, is an uncommon but clinically significant cause of complicated urinary tract infections (UTIs). Unlike typical uropathogens such as Escherichia coli, S. aureus presence in the urinary tract often signals systemic involvement, particularly hematogenous spread from a distant primary infection. Recognizing the pathogenic role of S. aureus in complicated UTIs is essential for prompt diagnosis, targeted therapy, and the prevention of life-threatening complications such as sepsis and endocarditis.
Pathogenesis: How Staphylococcus aureus Causes Complicated UTI
Hematogenous vs Ascending Spread
Unlike conventional UTIs, S. aureus frequently enters the urinary tract via the bloodstream (hematogenous seeding), especially in the context of bacteremia. This is more common in:
- Patients with intravascular catheters
- Those with prosthetic devices
- Individuals undergoing hemodialysis
- Patients with infective endocarditis
Ascending infections caused by S. aureus are rare but may occur in catheterized patients or those with structural urinary tract abnormalities.
Risk Factors Associated with S. aureus Complicated UTI
- Indwelling urinary catheters
- Immunosuppression (e.g., transplant, cancer, HIV)
- Recent urologic procedures
- Diabetes mellitus
- Hospitalization or ICU stay
- Presence of foreign bodies (e.g., stents, nephrostomy tubes)
- Chronic kidney disease or dialysis
- Prosthetic heart valves or pacemakers (associated with endocarditis)
Clinical Presentation and Symptoms
The clinical features of a complicated UTI due to S. aureus vary depending on the route of infection and systemic involvement. Common symptoms include:
- High-grade fever with chills
- Flank or abdominal pain
- Dysuria and frequency (less common in hematogenous cases)
- Hematuria
- Nausea and vomiting
- Malaise and sepsis
- Signs of pyelonephritis or renal abscess
- Back pain, particularly if vertebral osteomyelitis or epidural abscess is present
Diagnostic Approach to S. aureus in the Urinary Tract
The identification of S. aureus in urine warrants thorough investigation to differentiate between true infection and colonization or contamination. A structured diagnostic protocol includes:
Laboratory Tests
- Urine culture: Quantitative growth of S. aureus ≥10⁵ CFU/mL confirms infection
- Blood cultures: Essential to assess for concurrent bacteremia
- Urinalysis: Pyuria, leukocyte esterase, and nitrites may be present
- Inflammatory markers: Elevated CRP and ESR
- Serum creatinine: Assess renal function
Imaging Studies
- Renal ultrasound or CT urogram: Detects abscesses, obstruction, or anatomic abnormalities
- Echocardiography (TTE/TEE): To rule out endocarditis in cases of persistent bacteremia
- MRI spine: If vertebral involvement is suspected
Methicillin-Resistant Staphylococcus aureus (MRSA) and its Implications
MRSA UTIs are often associated with healthcare exposure and increased antibiotic resistance. These cases demand special attention due to:
- Higher risk of bacteremia and metastatic infections
- Limited antibiotic options
- Increased recurrence and mortality rates
Antibiotic therapy must be adjusted based on susceptibility profiles, often requiring intravenous agents for adequate renal parenchymal penetration.
Treatment Protocol for S. aureus Complicated UTI
Empiric and Targeted Antimicrobial Therapy
Methicillin-sensitive S. aureus (MSSA):
- Nafcillin or oxacillin (IV)
- Cefazolin (IV)
- Transition to oral cephalexin or dicloxacillin if clinically appropriate
Methicillin-resistant S. aureus (MRSA):
- Vancomycin (IV, serum level monitoring required)
- Linezolid (oral/IV, for cases with good oral tolerance)
- Daptomycin (not effective in lung infections but viable for bacteremic UTI)
Treatment Duration
- Uncomplicated bacteriuria: Rare, short course if symptomatic
- Complicated UTI with bacteremia: Minimum of 14 days of IV therapy
- Renal abscesses or endocarditis: 4–6 weeks of treatment depending on severity and source
Adjunctive Measures
- Removal or replacement of indwelling catheters
- Drainage of abscesses or obstructive uropathy
- Surgical intervention if prosthetic devices are the source
Complications of Untreated or Inadequately Treated Infections
Failure to recognize or fully treat S. aureus complicated UTIs can result in:
- Renal abscess formation
- Persistent bacteremia
- Infective endocarditis
- Vertebral osteomyelitis
- Septic emboli to distant organs
- Urosepsis and multiorgan dysfunction
Infection Control and Preventive Strategies
Hospital-Based Measures
- Strict hand hygiene compliance
- Aseptic catheter insertion and maintenance protocols
- Early catheter removal
- MRSA decolonization protocols in high-risk populations
Patient-Level Prevention
- Adequate hydration
- Timely management of urinary tract obstructions
- Glycemic control in diabetic patients
- Regular screening in high-risk settings such as dialysis units
Special Populations
Dialysis Patients
Staphylococcus aureus bacteriuria in hemodialysis patients often reflects systemic infection from vascular access. These cases require comprehensive systemic evaluation.
Geriatric Patients
Elderly individuals with functional or cognitive impairment are particularly susceptible due to chronic catheterization and immune senescence.
Pediatric Considerations
Pediatric S. aureus UTI is rare and often indicates congenital anomalies or hematogenous dissemination from skin infections.
Staphylococcus aureus complicated urinary tract infections demand an aggressive diagnostic and therapeutic approach. Unlike routine UTIs, these infections often reflect deeper systemic pathology, such as bacteremia or renal abscesses, and require extended antimicrobial therapy, imaging, and sometimes surgical intervention. Vigilant surveillance, timely catheter management, and prompt treatment are vital for optimal outcomes in this high-risk patient group.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will