Staphylococcus aureus is a gram-positive coccal bacterium that often colonizes the skin and mucosal surfaces. While it is part of the normal human flora, it becomes pathogenic when it invades sterile sites, particularly the respiratory tract. Bronchitis caused by S. aureus is relatively rare compared to viral forms but can lead to significant complications, especially in immunocompromised individuals or those with underlying lung diseases.
Causes and Risk Factors for Staphylococcal Bronchitis
Primary Causes
Staphylococcus aureus bronchitis can develop through:
- Aspiration of oropharyngeal flora during mechanical ventilation or poor swallowing reflex
- Hematogenous spread from a distant staph infection
- Colonization and subsequent infection in patients with chronic obstructive pulmonary disease (COPD), cystic fibrosis, or bronchiectasis
Risk Factors
- Recent hospitalization or ICU stay
- Chronic lung diseases
- Use of corticosteroids or immunosuppressants
- Structural lung damage
- Inhalation drug use
- Recent influenza or viral upper respiratory infection
- Presence of indwelling medical devices (e.g., ventilators)
Symptoms of Staphylococcus aureus Bronchitis
Clinical presentation of staphylococcal bronchitis may resemble other bacterial or viral respiratory infections, yet some features are more prominent in staph infections:
- Persistent, productive cough with purulent or blood-tinged sputum
- Fever and chills
- Shortness of breath
- Wheezing or chest tightness
- Pleuritic chest pain
- Malaise and fatigue
- Occasional hemoptysis
Methicillin-Resistant Staphylococcus aureus (MRSA) and Its Impact
Methicillin-resistant Staphylococcus aureus (MRSA) significantly complicates the treatment landscape. MRSA bronchitis often emerges in healthcare settings and is notoriously resistant to beta-lactam antibiotics.
Common Characteristics of MRSA Bronchitis:
- Higher fever and more aggressive symptoms
- Increased likelihood of systemic spread (e.g., pneumonia or septicemia)
- Poorer response to standard antibiotics
Diagnostic Evaluation
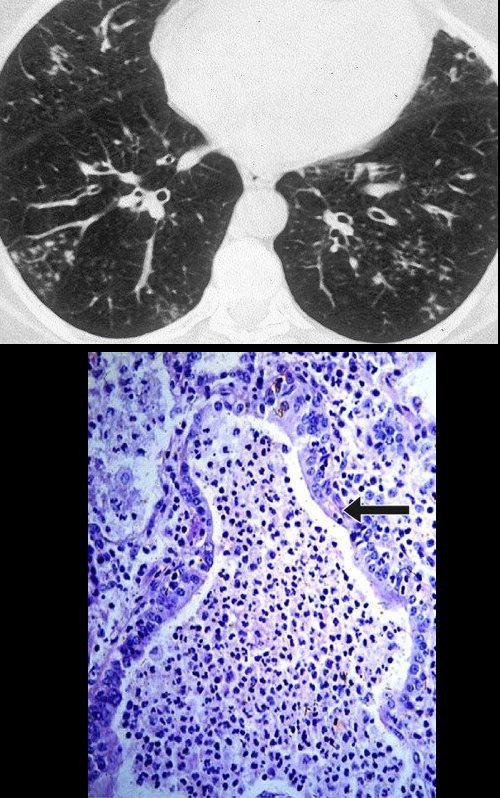
Laboratory and Imaging Investigations
Accurate diagnosis is essential for effective treatment. The following diagnostics are typically employed:
- Sputum Gram stain and culture to confirm S. aureus and determine resistance patterns
- Blood cultures to rule out bacteremia
- Chest X-ray or CT scan to identify consolidation, abscesses, or cavitary lesions
- Bronchoscopy with lavage in non-responders or ventilated patients
- PCR-based assays for rapid detection of MRSA strains
Treatment Strategies for Staphylococcus aureus Bronchitis
Antibiotic Therapy
Treatment must be tailored based on methicillin susceptibility:
- Methicillin-sensitive S. aureus (MSSA):
- Nafcillin or oxacillin
- First-generation cephalosporins (e.g., cefazolin)
- Methicillin-resistant S. aureus (MRSA):
- Vancomycin (IV)
- Linezolid (IV or oral)
- Daptomycin (not for pulmonary use due to surfactant inactivation)
- Clindamycin or doxycycline in less severe cases
Supportive Management
- Adequate hydration and mucolytics
- Bronchodilators for obstructive symptoms
- Oxygen therapy in hypoxemic patients
- Corticosteroids may be used cautiously in COPD exacerbations
- Chest physiotherapy to mobilize secretions
Complications and Prognosis
If left untreated or inadequately managed, S. aureus bronchitis may progress to:
- Necrotizing pneumonia
- Pulmonary abscess formation
- Empyema (pleural effusion with pus)
- Respiratory failure
- Sepsis and multiorgan dysfunction in severe MRSA cases
Prognosis is generally favorable in otherwise healthy individuals with early treatment but is guarded in elderly, immunocompromised, or ventilated patients.
Prevention and Infection Control
Preventive Measures
- Hand hygiene and contact precautions in hospital settings
- Decolonization protocols (e.g., intranasal mupirocin, chlorhexidine washes) for recurrent infections
- Influenza vaccination to prevent secondary bacterial bronchitis
- Smoking cessation to improve mucociliary clearance
- Avoidance of unnecessary antibiotic use to reduce resistance emergence
Staphylococcal Bronchitis in Special Populations
Pediatric Considerations
Children with cystic fibrosis are at increased risk of chronic colonization and infection with S. aureus. Prophylactic antibiotics and aggressive airway clearance are often warranted.
Immunocompromised Hosts
Patients with HIV/AIDS, organ transplants, or undergoing chemotherapy are susceptible to more severe and recurrent forms. Broad-spectrum antibiotics with MRSA coverage are usually indicated upfront in such populations.
Staphylococcus aureus bronchitis, though less common than viral forms, represents a serious clinical entity with potential for significant morbidity, especially in vulnerable patients. Early diagnosis, appropriate antimicrobial therapy, and supportive measures are critical in reducing complications and improving patient outcomes. Vigilant infection control and awareness of emerging resistant strains like MRSA remain central to containment and treatment success.