Staphylococcal enterocolitis is an under-recognized but clinically significant gastrointestinal condition caused by enterotoxin-producing strains of Staphylococcus aureus, typically following antibiotic therapy or in hospitalized patients. Characterized by severe diarrhea, abdominal discomfort, and systemic symptoms, this form of enterocolitis requires precise diagnosis and targeted treatment, particularly to differentiate it from Clostridioides difficile colitis.
Pathogenesis of Staphylococcal Enterocolitis
Disruption of Normal Gut Flora
The gastrointestinal microbiota plays a critical role in maintaining intestinal homeostasis. Broad-spectrum antibiotic therapy can significantly reduce microbial diversity, creating an environment conducive to colonization by pathogenic organisms such as S. aureus.
Role of Enterotoxins
Enterotoxigenic strains of S. aureus release heat-stable enterotoxins (most commonly enterotoxins A, B, and D) that induce mucosal inflammation, epithelial damage, and secretory diarrhea. These toxins act as superantigens, leading to extensive immune activation and inflammation of the colonic mucosa.
Epidemiology and Risk Factors
Staphylococcal enterocolitis is most frequently seen in:
- Postoperative patients (especially gastrointestinal surgeries)
- Individuals receiving broad-spectrum antibiotics
- Hospitalized or ICU patients
- Elderly or immunocompromised individuals
- Patients with nasogastric tubes or prolonged NPO status
Nosocomial outbreaks have been documented, often involving methicillin-resistant S. aureus (MRSA) strains.
Clinical Presentation of Staph-Induced Enterocolitis
The condition typically manifests within days of antibiotic exposure or hospitalization, with the following symptoms:
- Profuse watery diarrhea, often without blood
- Abdominal pain or cramping
- Fever and chills
- Nausea or vomiting
- Signs of dehydration
- Leukocytosis with elevated neutrophils
Notably, unlike C. difficile, staphylococcal enterocolitis may not produce pseudomembranes or overtly foul-smelling stools, making clinical differentiation challenging without laboratory confirmation.
Diagnostic Criteria and Laboratory Evaluation
Stool Studies
- Stool culture for S. aureus (both MSSA and MRSA)
- Toxin detection assays to confirm enterotoxin presence (via ELISA or PCR)
- Rule out Clostridioides difficile toxin A/B
- Fecal leukocytes and elevated fecal calprotectin may indicate inflammation
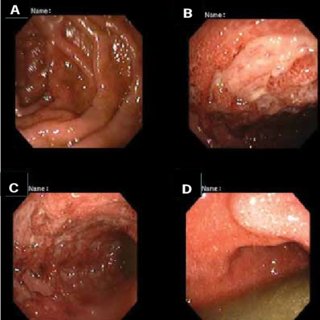
Endoscopic Evaluation
Flexible sigmoidoscopy or colonoscopy may reveal:
- Diffuse colonic erythema
- Mucosal edema
- Absence of pseudomembranes (in contrast to C. difficile)
Additional Tests
- Blood cultures in febrile or septic patients
- Electrolytes and renal function tests to assess dehydration
- Imaging (CT abdomen) if complications such as toxic megacolon or perforation are suspected
Differential Diagnosis
It is essential to distinguish staphylococcal enterocolitis from other infectious and inflammatory conditions:
- Clostridioides difficile infection
- Inflammatory bowel disease
- Viral gastroenteritis (e.g., norovirus)
- Ischemic colitis
- Campylobacter, Salmonella, Shigella enterocolitis
Failure to identify S. aureus as the etiologic agent can result in ineffective treatment and prolonged illness.
Treatment Strategies for Staphylococcal Enterocolitis
Antibiotic Therapy
Treatment is targeted based on culture and sensitivity results:
- Oral vancomycin or linezolid for MRSA strains
- Clindamycin, rifaximin, or trimethoprim-sulfamethoxazole for MSSA strains
- Discontinuation of inciting broad-spectrum antibiotics is essential
Supportive Measures
- Aggressive fluid and electrolyte replacement
- Bowel rest in cases of severe symptoms
- Probiotic supplementation (under clinical guidance)
Infection Control
In cases of nosocomial outbreaks:
- Contact precautions
- Decolonization of MRSA carriers
- Environmental disinfection
Complications of Untreated or Delayed Management
- Hypovolemia and electrolyte imbalance
- Bacteremia and sepsis
- Toxic megacolon
- Recurrence or chronic diarrhea
- Secondary infections due to disrupted gut mucosa
Timely intervention and microbiological diagnosis significantly improve outcomes and reduce the risk of systemic spread.
Preventive Measures and Hospital Guidelines
- Antimicrobial stewardship to reduce unnecessary antibiotic exposure
- Hand hygiene protocols in hospital settings
- Regular surveillance cultures in ICUs
- Isolating infected or colonized patients to prevent cross-contamination
Additionally, awareness among clinicians about S. aureus as a cause of nosocomial diarrhea is crucial for appropriate diagnostic testing and management.
Frequently Asked Questions
Is staphylococcal enterocolitis the same as food poisoning?
No. While both may be caused by S. aureus enterotoxins, food poisoning is typically acute and self-limiting, whereas enterocolitis occurs in hospitalized or antibiotic-exposed patients and may require targeted antibiotic therapy.
How is staphylococcal enterocolitis different from C. difficile colitis?
C. difficile typically presents with pseudomembranous colitis, a foul stool odor, and is confirmed via toxin assays. Staphylococcal enterocolitis lacks pseudomembranes and is confirmed via stool culture and toxin assays for S. aureus.
Can it resolve without antibiotics?
Mild cases may improve with withdrawal of the inciting antibiotic and supportive care. However, MRSA-associated cases usually require specific antibiotics to prevent complications.
Is recurrence common?
Recurrence is possible, particularly in patients who remain immunosuppressed, hospitalized, or continue to receive broad-spectrum antibiotics. Decolonization and infection control are vital in prevention.
Staphylococcal enterocolitis is a serious gastrointestinal infection that requires heightened clinical suspicion, especially in hospitalized patients with recent antibiotic exposure. Differentiation from other enteric infections such as C. difficile is critical, as misdiagnosis can delay effective treatment. Targeted antimicrobial therapy, supportive care, and robust infection control practices form the cornerstone of effective management. Awareness and early detection are key to reducing morbidity and preventing nosocomial transmission.