Staphylococcus aureus is a Gram-positive bacterium that commonly colonizes the skin and mucous membranes. When the skin barrier is compromised due to trauma, such as cuts, abrasions, lacerations, or surgical wounds, S. aureus can invade underlying tissues, leading to localized or systemic infections. These infections range in severity from mild superficial lesions to life-threatening sepsis, particularly in immunocompromised individuals or those with chronic illnesses.
Understanding Staph Aureus as a Pathogen in Skin Trauma
Staphylococcus aureus thrives on the skin but becomes pathogenic when it penetrates the epidermis. In traumatic skin injuries, the protective barrier is breached, allowing opportunistic colonization by S. aureus. Methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant Staphylococcus aureus (MRSA) are both capable of causing serious infections, with MRSA posing significant treatment challenges due to antibiotic resistance.
Risk Factors for Staph Aureus Infection After Skin Trauma
- Open wounds or lacerations
- Poor wound hygiene
- Previous colonization with S. aureus or MRSA
- Immunosuppression (e.g., HIV, diabetes, cancer)
- Hospitalization or recent surgery
- Close skin-to-skin contact in high-density environments (e.g., athletes, military)
- Use of contaminated medical devices or dressings
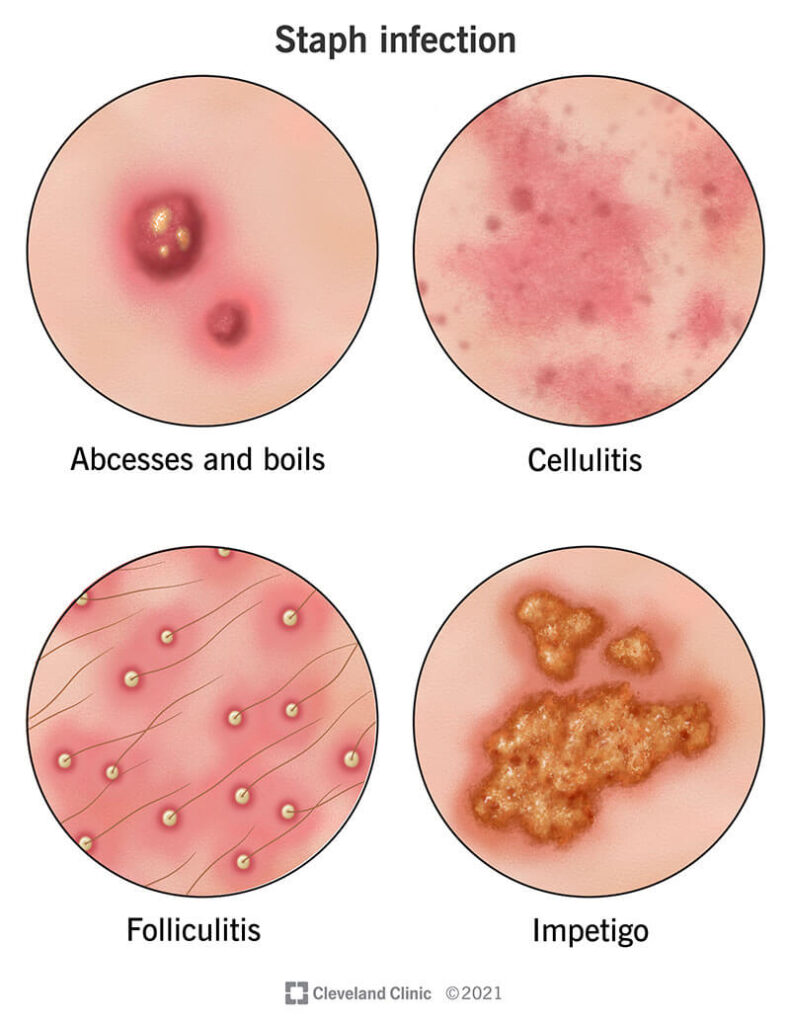
Clinical Manifestations of Traumatic Staph Skin Infections
Localized Infections
- Erythema and swelling around the wound site
- Painful pustules or boils
- Formation of abscesses with purulent drainage
- Crusting or yellow exudate at the site
- Delayed wound healing
Spreading Infections
- Cellulitis: Warm, red, tender swelling extending beyond the wound margin
- Lymphangitis: Red streaks indicating lymphatic spread
- Fever and malaise in more extensive infections
Systemic Complications
- Bacteremia: Entry of S. aureus into the bloodstream
- Sepsis: Systemic inflammatory response with hypotension, organ dysfunction
- Endocarditis or osteomyelitis in cases of hematogenous spread
Diagnostic Workup for Staph Aureus Wound Infection
Physical Examination
The appearance of the lesion, presence of purulence, and signs of systemic illness guide clinical suspicion. Rapid progression of erythema or tissue necrosis requires urgent evaluation.
Microbiological Testing
- Wound culture and sensitivity: Essential for identifying S. aureus and determining antibiotic susceptibility, particularly to distinguish MRSA from MSSA.
- Blood cultures: Recommended in febrile patients or those showing systemic symptoms.
- PCR and molecular diagnostics: May be used for rapid MRSA detection.
Imaging
- Ultrasound: Useful to detect subcutaneous abscesses.
- MRI or CT: Indicated if deep tissue involvement or osteomyelitis is suspected.
Treatment Options for Staphylococcus Aureus Skin Infections
Localized Infections (without systemic involvement)
Incision and Drainage
- Primary treatment for abscesses. Often sufficient for small, uncomplicated lesions.
Topical Antibiotics
- Mupirocin or fusidic acid may be applied to minor lesions or used for decolonization in recurrent infections.
Oral Antibiotics
- For MSSA: Dicloxacillin, cephalexin
- For MRSA: Clindamycin, doxycycline, TMP-SMX (based on culture results)
Moderate to Severe Infections
Intravenous Antibiotics
- For MSSA: Nafcillin, oxacillin, or cefazolin
- For MRSA: Vancomycin, linezolid, daptomycin, or ceftaroline
Hospitalization
Required for:
- Rapid progression of infection
- High fever or systemic involvement
- Immunocompromised status
- Failure of oral antibiotics
Prevention and Wound Care for Traumatic Lesions
Wound Hygiene
- Immediate cleansing with saline or antiseptic solution
- Avoidance of occlusive dressings if pus is present
- Frequent dressing changes under aseptic conditions
Decolonization Protocols
For individuals with recurrent infections:
- Nasal mupirocin twice daily for 5 days
- Chlorhexidine washes for 7 days
- Environmental decontamination (linens, personal items)
Vaccination and Research
There is ongoing research into vaccines against S. aureus, though no licensed vaccine exists as of now. Preventive strategies are focused on hygiene and limiting antibiotic overuse.
Antibiotic Resistance and the Challenge of MRSA
Methicillin-resistant Staphylococcus aureus has become a major public health concern. Resistance arises from the mecA gene, which alters penicillin-binding proteins and renders β-lactam antibiotics ineffective. Community-acquired MRSA (CA-MRSA) strains often produce Panton-Valentine leukocidin (PVL) toxin, associated with tissue necrosis and severe infections.
Effective MRSA control requires:
- Judicious antibiotic use
- Targeted decolonization strategies
- Rigorous hand hygiene and environmental cleaning
- Contact precautions in healthcare settings
Complications of Untreated or Mismanaged Infections
- Chronic ulcers or delayed healing
- Necrotizing fasciitis
- Septic arthritis or osteomyelitis
- Endocarditis in bacteremic patients
- Toxic shock syndrome, especially in cases involving toxin-producing strains
Prompt recognition and appropriate management are vital to prevent long-term morbidity or mortality associated with invasive staphylococcal infections.
Frequently Asked Questions
How can I tell if my cut is infected with Staph aureus?
Signs include increasing redness, swelling, warmth, pain, pus drainage, and failure to heal. Seek medical attention if fever or spreading redness develops.
What should I do if I suspect MRSA?
Cover the wound, avoid contact with others, and consult a healthcare provider for culture and appropriate antibiotics.
Can I prevent a traumatic wound from becoming infected?
Yes. Clean the wound immediately, keep it covered with sterile dressings, and monitor for signs of infection. Practice good hygiene and avoid touching the wound.
Are antibiotics always needed?
Not always. Small abscesses may resolve with drainage alone. However, antibiotics are crucial for spreading infections, systemic symptoms, or immunocompromised patients.
Staphylococcus aureus remains a leading cause of infection in traumatic skin lesions, with clinical outcomes ranging from minor abscesses to life-threatening systemic complications. Prompt diagnosis, appropriate antimicrobial therapy, surgical drainage when necessary, and adherence to infection prevention protocols are essential. With growing concerns over MRSA, effective treatment strategies must balance antibiotic stewardship with the need to address severe infections decisively. Prevention through hygiene, education, and wound care remains the cornerstone of reducing the burden of staphylococcal skin infections.

