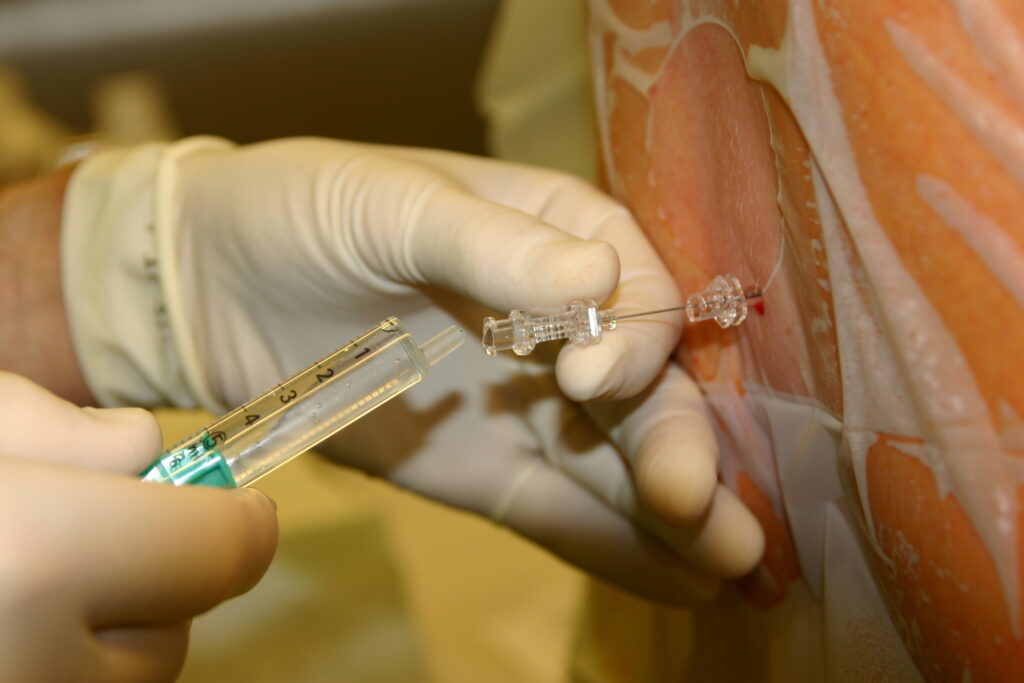
Spinal anesthesia, also known as subarachnoid block or spinal block, is a form of regional anesthesia that involves injecting a local anesthetic into the subarachnoid space of the spinal cord. It is widely employed in lower abdominal, pelvic, and lower extremity surgeries due to its rapid onset, predictable effect, and minimized systemic involvement. A meticulous understanding of spinal anesthesia is essential for safe administration and optimal patient outcomes.
Anatomy and Mechanism of Spinal Anesthesia
Spinal anesthesia exerts its effect by blocking nerve conduction in the spinal cord and nerve roots, particularly targeting sensory, motor, and sympathetic nerves.
Targeted Region
- Subarachnoid space: Between the arachnoid mater and pia mater
- Typical insertion site: Between L3–L4 or L4–L5, below the termination of the spinal cord to avoid neurological injury
Indications for Spinal Anesthesia
Spinal anesthesia is selected based on the nature of the surgery, patient health status, and desired level of nerve block.
Common Indications
- Cesarean sections and gynecological procedures
- Urologic surgeries (e.g., TURP)
- Lower limb orthopedic operations
- Hernia repairs
- Perineal and anorectal surgeries
Contraindications
- Absolute:
- Patient refusal
- Increased intracranial pressure
- Infection at the injection site
- Severe hypovolemia
- Relative:
- Coagulopathy or anticoagulant use
- Neurological disorders
- Spinal deformities
Step-by-Step Spinal Anesthetic Procedure
Pre-procedure Preparation
- Informed consent
- IV access and fluid preload to prevent hypotension
- Positioning: Either sitting or lateral decubitus
Technique
- Aseptic technique and skin preparation
- Local anesthesia at the puncture site
- Introduction of a spinal needle (usually 25G–27G)
- Identification of CSF return confirms subarachnoid placement
- Injection of local anesthetic (e.g., bupivacaine, lidocaine)
Monitoring
- Vital signs every 5 minutes during onset
- Assessment of block level (sensory and motor)
Commonly Used Spinal Anesthetic Agents
| Drug | Onset (min) | Duration (min) | Notable Features |
|---|---|---|---|
| Bupivacaine | 5–8 | 90–180 | Long duration, widely used |
| Lidocaine | 2–5 | 60–90 | Rapid onset, shorter surgeries |
| Ropivacaine | 5–10 | 90–150 | Less cardiotoxic than bupivacaine |
| Tetracaine | 5–10 | 120–240 | Preferred for long duration cases |
Benefits and Advantages of Spinal Anesthesia
- Rapid onset and effective sensory/motor block
- Reduced systemic drug exposure
- Lower risk of thromboembolism and pulmonary complications
- Awake patient with stable hemodynamics
- Minimal postoperative nausea and vomiting
Potential Complications and Management
Common Side Effects
- Hypotension and bradycardia
- Post-dural puncture headache (PDPH)
- Urinary retention
- Nausea and vomiting
Rare but Serious Complications
- Neurological damage
- Infection (meningitis or abscess)
- Spinal hematoma
Prevention and Management Strategies
| Complication | Prevention | Treatment |
|---|---|---|
| Hypotension | IV fluids preload | Vasopressors (e.g., phenylephrine) |
| PDPH | Use of fine gauge needle | Caffeine, hydration, epidural blood patch |
| Urinary retention | Monitor bladder function | Catheterization if necessary |
Comparison with Epidural Anesthesia
| Feature | Spinal Anesthesia | Epidural Anesthesia |
|---|---|---|
| Injection Site | Subarachnoid space | Epidural space |
| Onset | Rapid | Slower |
| Catheter Placement | No | Yes |
| Duration Control | Limited | Adjustable |
| Drug Volume | Low | High |
Spinal anesthesia is often preferred for shorter and more definitive procedures, while epidural anesthesia allows for continuous and adjustable dosing, making it suitable for labor or prolonged surgeries.
Recovery and Postoperative Care
- Monitor block regression: Sensory and motor return
- Pain management: Transition to systemic analgesics
- Mobilization: Encourage early ambulation when feasible
- Hydration and bladder care: Prevent complications like retention or hypotension
Most patients recover full neurological function within a few hours, and residual symptoms like mild headache or transient numbness typically resolve without intervention.
Spinal Anesthesia in Special Populations
Obstetric Use
- Preferred method for cesarean section
- Minimizes fetal drug exposure
- Allows mother to remain awake and participate in birth
Elderly Patients
- Dose adjustments required due to decreased CSF volume
- Enhanced sensitivity to anesthetics
- Close monitoring for hypotension and bradycardia
Patients on Anticoagulants
- Require careful assessment of clotting parameters
- Adhere strictly to ASRA guidelines to minimize hematoma risk
Frequently Asked Questions
How long does spinal anesthesia last?
Duration varies with the drug used but typically ranges from 1.5 to 4 hours.
Is spinal anesthesia safer than general anesthesia?
For appropriate procedures, spinal anesthesia offers fewer respiratory complications, faster recovery, and better postoperative pain control.
Can spinal anesthesia cause paralysis?
Permanent paralysis is extremely rare, especially when proper technique and precautions are followed.
What does spinal anesthesia feel like?
Patients may feel numbness, warmth, or heaviness in the legs, without pain or movement ability during the surgery.
Spinal anesthesia remains a cornerstone of regional anesthetic practice, offering profound sensory and motor blockade with minimal systemic effects. Its utility in obstetrics, orthopedics, and urology is well-established. With precise technique, appropriate patient selection, and vigilant monitoring, spinal anesthesia provides a safe, efficient, and patient-centered alternative to general anesthesia.