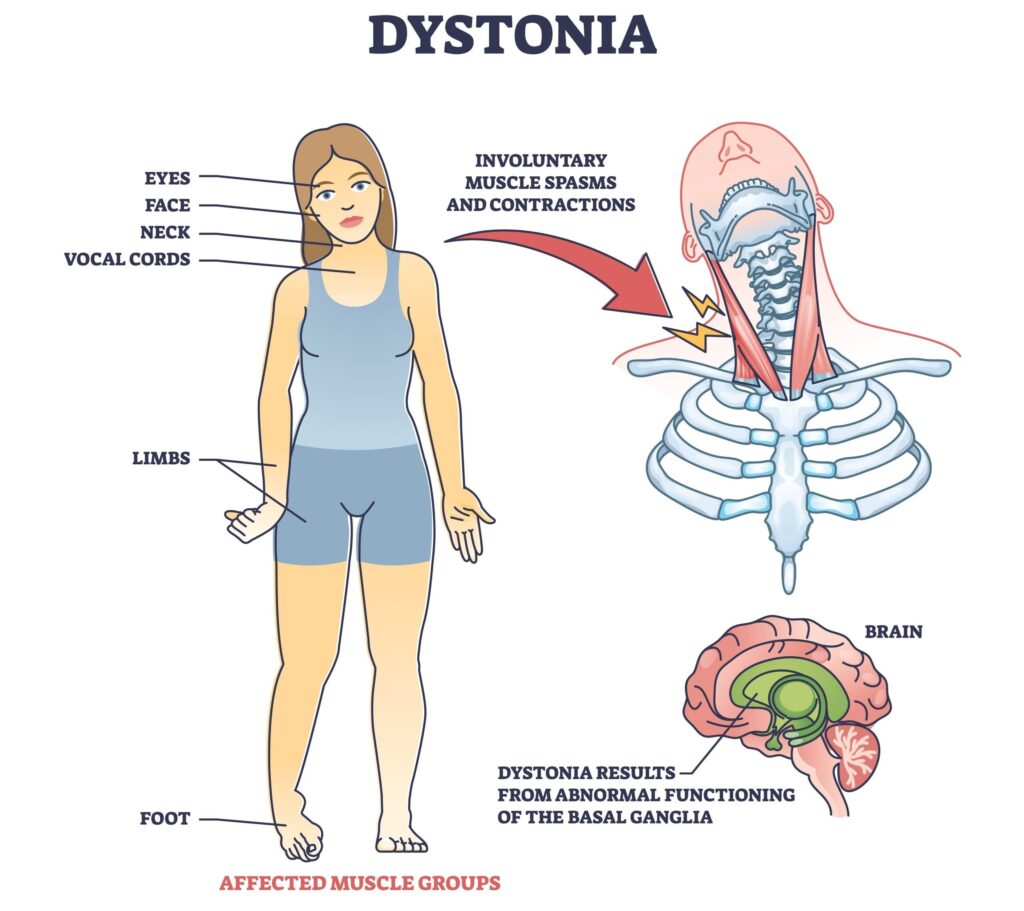
Spasmodic torticollis, also known as cervical dystonia, is a chronic neurological movement disorder characterized by involuntary muscle contractions in the neck. These contractions cause abnormal movements and postures of the head and neck, often resulting in significant discomfort, functional limitations, and psychological distress. While the precise cause remains elusive in many cases, advances in diagnostic techniques and treatment modalities have significantly improved symptom management and patient quality of life.
Causes and Risk Factors of Spasmodic Torticollis
Primary vs. Secondary Torticollis
Spasmodic torticollis may be classified as:
- Primary (Idiopathic): No identifiable structural lesion; often genetic or spontaneous.
- Secondary: Attributed to underlying causes such as trauma, stroke, infections, or medication side effects (e.g., antipsychotics causing tardive dystonia).
Contributing Factors
- Genetic predisposition
- Head or neck trauma
- Neurodegenerative diseases
- Prolonged use of dopamine-blocking agents
- Psychological stress, which may exacerbate symptoms
Recognizing the Symptoms of Spasmodic Torticollis
Common Clinical Presentations
- Intermittent or sustained involuntary neck muscle contractions
- Abnormal head positions, such as:
- Rotational torticollis (head turns to one side)
- Laterocollis (head tilts to one side)
- Retrocollis (head tilts backward)
- Anterocollis (head tilts forward)
Associated Features
- Neck pain and stiffness
- Tremor or jerking head movements
- Hypertrophy of neck muscles
- Fatigue or discomfort exacerbated by stress or activity
Diagnostic Process for Cervical Dystonia
Accurate diagnosis is essential for effective treatment. While diagnosis is primarily clinical, further evaluation may be necessary to rule out secondary causes.
Clinical Tools
- Physical exam: Observation of movement patterns
- Electromyography (EMG): Evaluates muscle activity
- Neuroimaging (MRI/CT): Identifies structural abnormalities
- Genetic testing: In familial or early-onset cases
Treatment Options for Spasmodic Torticollis
Botulinum Toxin Injections
First-line therapy for most patients:
- Administered into overactive neck muscles
- Reduces muscle contractions and pain
- Effects typically last 12–16 weeks
- Requires repeat injections
Commonly used formulations:
- OnabotulinumtoxinA (Botox)
- AbobotulinumtoxinA (Dysport)
- IncobotulinumtoxinA (Xeomin)
Oral Medications
Used in conjunction with botulinum toxin or in refractory cases:
- Anticholinergics (e.g., trihexyphenidyl)
- Benzodiazepines (e.g., clonazepam)
- Muscle relaxants (e.g., baclofen)
Physical Therapy and Supportive Care
- Stretching exercises
- Postural training
- Biofeedback and relaxation techniques
- Heat therapy and massage
Surgical Interventions
Considered in severe, medication-refractory cases:
- Selective denervation surgery (e.g., the Bertrand procedure)
- Deep Brain Stimulation (DBS): Effective in generalized or segmental dystonia
Prognosis and Long-Term Outlook
Spasmodic torticollis is a chronic but manageable condition. While a complete cure remains elusive, most patients experience significant improvement with appropriate therapy. The condition does not typically affect life expectancy but can cause:
- Chronic pain
- Social embarrassment
- Reduced productivity and quality of life
Early diagnosis and multidisciplinary treatment yield the best outcomes.
Living with Spasmodic Torticollis: Coping and Support
Lifestyle Strategies
- Stress management: Stress often worsens symptoms
- Ergonomic adjustments: Chairs with neck support, mirror placement
- Sleep hygiene: Proper pillow support to reduce nocturnal discomfort
Emotional and Social Support
- Joining support groups (in-person or online)
- Consulting mental health professionals for depression or anxiety
- Building a strong family and caregiver network
Frequently Asked Questions
What triggers spasmodic torticollis?
Triggers vary but commonly include stress, fatigue, or specific head movements. In some cases, there is no identifiable trigger.
Is cervical dystonia hereditary?
While most cases are sporadic, a minority may have a genetic component, especially if onset occurs before age 30.
Can exercise help with spasmodic torticollis?
Yes, physical therapy and guided exercises improve posture, reduce pain, and increase mobility.
How often are botulinum toxin injections needed?
Injections are usually repeated every 3 to 4 months, depending on the individual response and symptom recurrence.
Is spasmodic torticollis curable?
There is no definitive cure, but long-term symptom control is achievable through a combination of medical and rehabilitative therapies.
Spasmodic torticollis is a complex neurological disorder marked by involuntary contractions of the neck muscles, leading to abnormal postures and functional impairment. With prompt diagnosis, tailored botulinum toxin therapy, supportive medications, and rehabilitative care, most individuals can achieve meaningful relief and maintain a good quality of life. Continued research into the pathophysiology and novel treatment modalities offers hope for further advancements in care.