Abdominal colic refers to a severe, intermittent pain in the abdomen, often resulting from spasms or obstructions in the hollow organs, such as the intestines, biliary tract, or urinary tract. This condition affects individuals across all age groups and requires careful evaluation to identify its underlying cause.
Understanding the etiology, clinical features, diagnostic methods, and treatment options is critical for effective management and improving patient outcomes.
Causes of Abdominal Colic
The underlying causes of abdominal colic are diverse, ranging from benign to potentially life-threatening conditions. Some of the most common causes include:
1. Gastrointestinal Causes
- Bowel Obstruction: Mechanical blockage in the intestines due to adhesions, tumors, or hernias.
- Irritable Bowel Syndrome (IBS): Characterized by cramping pain associated with bowel habit changes.
- Intussusception: Telescoping of one part of the intestine into another, particularly in children.
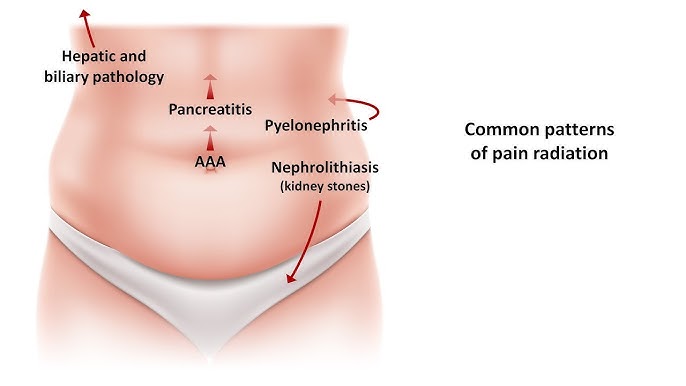
- Gallstones: Blockage of the bile ducts, leading to biliary colic.
- Appendicitis: Inflammation of the appendix, presenting with localized colicky pain.
2. Renal Causes
- Kidney Stones: Migration of stones through the urinary tract can cause excruciating colicky pain.
- Urinary Tract Obstruction: Conditions such as ureteric strictures or tumors.
3. Gynecological Causes
- Ovarian Cysts: Rupture or torsion can present with acute abdominal pain.
- Endometriosis: Pelvic pain due to ectopic endometrial tissue.
- Ectopic Pregnancy: A medical emergency requiring prompt diagnosis.
4. Other Causes
- Mesenteric Ischemia: Reduced blood flow to the intestines, often in older adults.
- Porphyria: A rare metabolic disorder causing abdominal pain.
- Infections: Gastroenteritis or parasitic infections such as ascariasis.
Clinical Features
The hallmark of abdominal colic is intermittent, cramping pain that varies in intensity. Other associated symptoms depend on the underlying cause and may include:
- Nausea and Vomiting: Common in gastrointestinal or renal causes.
- Fever: Suggestive of infections or inflammatory conditions.
- Changes in Bowel Habits: Diarrhea or constipation in IBS or bowel obstruction.
- Hematuria: Blood in urine in cases of kidney stones.
The pain is often localized but can radiate, such as to the back in biliary or renal colic.
Diagnostic Approach
A thorough history, physical examination, and targeted investigations are essential for diagnosing abdominal colic.
1. Clinical Evaluation
- History: Onset, duration, and nature of the pain, along with associated symptoms.
- Examination: Inspection, palpation, percussion, and auscultation to detect masses, tenderness, or abnormal bowel sounds.
2. Imaging Studies
- Ultrasound: Useful for detecting gallstones, kidney stones, or gynecological issues.
- Computed Tomography (CT): High sensitivity for bowel obstructions, appendicitis, and urinary tract stones.
- X-ray: Can reveal air-fluid levels in bowel obstruction or free air in cases of perforation.
- MRI: Preferred in pregnancy or for soft tissue evaluation.
3. Laboratory Tests
- Complete Blood Count (CBC): Elevated white blood cell count indicates infection or inflammation.
- Liver Function Tests (LFTs): Abnormal in biliary colic.
- Urinalysis: Detects hematuria or signs of infection.
- Amylase and Lipase: Elevated in pancreatitis.
Management Strategies
Management of abdominal colic involves addressing the underlying cause and providing symptomatic relief.
1. Medical Management
- Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids for pain relief.
- Antispasmodics: Reduce smooth muscle spasms in conditions like IBS or biliary colic.
- Antibiotics: Necessary for infections such as appendicitis or pyelonephritis.
2. Surgical Intervention
- Indicated in emergencies such as bowel obstruction, perforation, or ectopic pregnancy.
- Procedures may include laparotomy or laparoscopy for diagnosis and treatment.
3. Lifestyle Modifications
- Dietary Changes: Low-fat diet for biliary colic, high-fiber diet for IBS.
- Hydration: Prevents stone formation in the urinary tract.
Prevention and Risk Mitigation
Preventive measures focus on reducing risk factors associated with common causes of abdominal colic:
- Regular Screening: For individuals with a history of gallstones or urinary stones.
- Hydration: Adequate fluid intake to prevent renal stones.
- Dietary Adjustments: Balanced diet to maintain gastrointestinal and metabolic health.
- Avoid Prolonged IUD Use: Regular monitoring for complications in users.
Prognosis and Long-Term Outcomes
The prognosis of abdominal colic largely depends on the underlying condition and timeliness of intervention. While many cases resolve with appropriate treatment, delayed diagnosis or management can lead to complications such as:
- Sepsis: From untreated infections.
- Bowel Perforation: Due to delayed treatment of obstructions.
- Chronic Pain: Seen in conditions like endometriosis or recurrent stones.
Abdominal colic is a multifaceted condition that demands a systematic approach for accurate diagnosis and effective management. Timely identification of the underlying cause and appropriate intervention can significantly improve patient outcomes and prevent complications.