Obstructive Sleep Apnea (OSA) is a prevalent and serious sleep disorder characterized by repeated interruptions in breathing during sleep. One of the most debilitating symptoms is excessive daytime sleepiness, which can significantly impair quality of life, productivity, and safety. This article delves into the mechanisms behind OSA-induced sleepiness, diagnostic criteria, and effective treatment options.
What Causes Excessive Daytime Sleepiness in Obstructive Sleep Apnea?
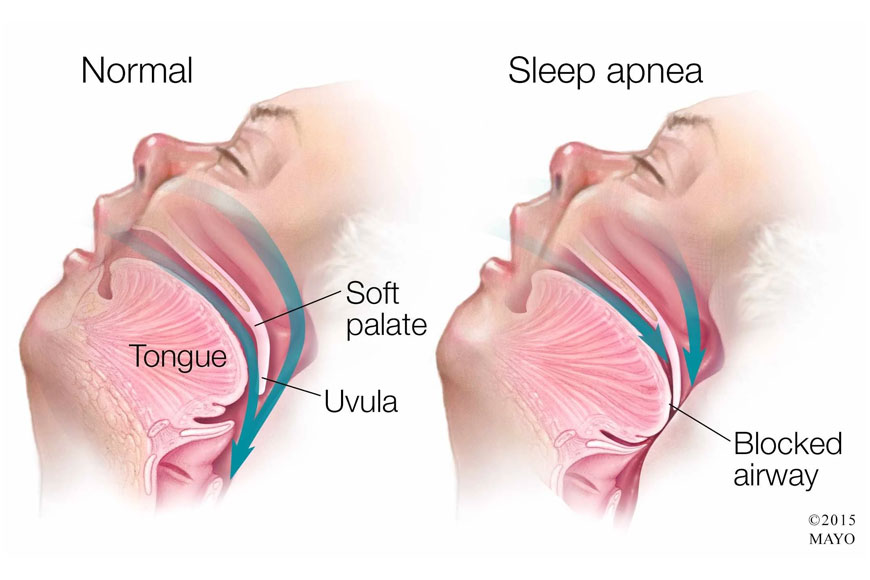
Obstructive sleep apnea occurs when the muscles at the back of the throat fail to keep the airway open, despite the effort to breathe. These obstructions lead to frequent arousals throughout the night, fragmenting sleep architecture and diminishing the restorative quality of rest. As a result, individuals experience:
- Decreased REM sleep, which is crucial for cognitive functioning
- Interrupted slow-wave sleep, responsible for physical restoration
- Sympathetic nervous system overactivation, contributing to poor sleep depth
This sleep fragmentation leads to chronic sleep debt, causing persistent fatigue, reduced alertness, and excessive daytime sleepiness.
Clinical Presentation: Recognizing Sleepiness in OSA Patients
Sleepiness due to obstructive sleep apnea often manifests in subtle yet progressive ways. Patients may initially report mild fatigue but gradually develop symptoms that affect both cognitive and physical functioning.
Common symptoms include:
- Falling asleep during passive activities (e.g., watching TV)
- Difficulty concentrating or memory lapses
- Poor work performance and frequent errors
- Increased irritability or mood changes
- Risk of drowsy driving or workplace accidents
Diagnostic Evaluation of Obstructive Sleep Apnea-Related Sleepiness
Diagnosing OSA and the resulting daytime sleepiness involves a multi-faceted approach. Evaluation typically includes:
1. Clinical History and Questionnaires
Standardized tools like the Epworth Sleepiness Scale (ESS) quantify sleepiness. Scores above 10 suggest excessive sleepiness requiring further evaluation.
2. Polysomnography (Sleep Study)
The gold standard in diagnosis, polysomnography records physiological data during sleep to assess apnea-hypopnea index (AHI). An AHI above 5 with symptoms confirms OSA.
3. Home Sleep Apnea Testing (HSAT)
For patients without significant comorbidities, HSAT offers a convenient and cost-effective diagnostic alternative, albeit with limited data compared to in-lab studies.
How Sleep Apnea-Induced Sleepiness Impacts Daily Functioning
Daytime sleepiness associated with obstructive sleep apnea can have far-reaching consequences:
- Cognitive Decline: Impaired attention, memory, and executive function
- Cardiovascular Risk: Increased likelihood of hypertension, stroke, and arrhythmia
- Metabolic Dysfunction: Poor glycemic control in diabetics
- Psychological Impact: Greater prevalence of depression and anxiety
- Social Consequences: Strain on relationships due to mood changes and fatigue
Treatment Strategies to Resolve Sleepiness in OSA Patients
Addressing the root cause of sleepiness—apneic events—is essential for symptom resolution. Treatment plans should be individualized based on severity and patient tolerance.
Continuous Positive Airway Pressure (CPAP)
CPAP therapy remains the most effective treatment, delivering pressurized air to keep the airway open during sleep. Adherence significantly reduces apneic events and improves daytime alertness.
Oral Appliance Therapy
For mild to moderate OSA or CPAP-intolerant patients, mandibular advancement devices reposition the jaw to maintain airway patency.
Lifestyle Modifications
- Weight loss reduces airway obstruction
- Positional therapy prevents supine-related apneas
- Alcohol and sedative avoidance lowers risk of airway collapse
Surgical Interventions
Options like uvulopalatopharyngoplasty (UPPP) or hypoglossal nerve stimulation may be considered for anatomical obstructions unresponsive to conservative measures.
Long-Term Outlook and Prognosis
When treated effectively, most patients experience a significant reduction in daytime sleepiness, improved quality of life, and lower risk of associated comorbidities. Untreated OSA, however, can lead to progressive neurocognitive decline and heightened mortality risk.
Sleepiness due to obstructive sleep apnea is a hallmark symptom of disrupted nighttime breathing. Early recognition and evidence-based treatment are essential for mitigating its cognitive, emotional, and physical consequences. Interdisciplinary care—including pulmonologists, sleep specialists, and behavioral therapists—offers the best outcomes for patients battling this silent yet profound disorder.

