Streptococcus species are among the most common causative agents of skin and skin structure infections (SSSIs). These infections range from mild impetigo to life-threatening necrotizing fasciitis. The most clinically significant species include Streptococcus pyogenes (Group A Streptococcus), Streptococcus agalactiae (Group B), and viridans group streptococci.
These pathogens often exploit compromised skin barriers to invade tissue, leading to inflammation, tissue necrosis, and systemic complications.
Epidemiology and Risk Profile of Streptococcal SSSIs
Streptococcal skin infections are prevalent in both community and healthcare settings. Group A Streptococcus (GAS) is the leading cause, responsible for over 10 million cases annually worldwide.
High-Risk Populations:
- Elderly adults
- Diabetics
- Immunocompromised individuals (e.g., HIV, chemotherapy patients)
- Patients with venous insufficiency or lymphedema
- Individuals with chronic wounds or skin conditions
- Residents in crowded environments (e.g., military, long-term care)
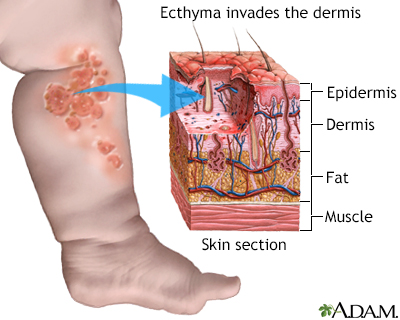
Clinical Manifestations of Streptococcal Skin Infections
Streptococcal infections present across a clinical spectrum. Recognition of early signs is critical to avoid complications.
Common Presentations:
| Condition | Characteristics |
|---|---|
| Impetigo | Superficial lesions with honey-colored crust, common in children |
| Erysipelas | Bright red, raised, well-demarcated rash, typically on face or legs |
| Cellulitis | Diffuse swelling, redness, warmth, and tenderness with indistinct borders |
| Necrotizing Fasciitis | Rapidly progressing pain, skin necrosis, systemic toxicity, requiring urgent surgery |
| Wound/Ulcer Infections | Purulent drainage, foul odor, delayed healing, often polymicrobial |
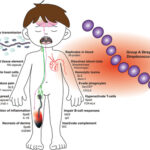
Virulence Factors Contributing to Streptococcal Pathogenicity
Streptococcal species possess numerous virulence determinants that facilitate colonization, immune evasion, and tissue destruction.
- M protein: Anti-phagocytic surface protein promoting adherence
- Streptolysins (O and S): Hemolysins that lyse host cells
- Exotoxins (SpeA, SpeB): Superantigens associated with toxic shock and necrotizing fasciitis
- Hyaluronidase and streptokinase: Enzymes enabling spread through connective tissues
Diagnostic Evaluation of Streptococcal SSSIs
A thorough clinical and microbiological assessment is essential for confirming streptococcal involvement and guiding treatment.
Diagnostic Components:
- Physical Examination: Identify signs of inflammation, necrosis, or systemic illness
- Culture and Sensitivity Testing:
- Wound swabs, aspirates, or biopsy for Gram stain and culture
- Blood cultures in severe or systemic infections
- Laboratory Tests:
- Leukocytosis and elevated C-reactive protein (CRP)
- Creatine kinase (CK) in suspected necrotizing fasciitis
- Imaging:
- Ultrasound to rule out abscess
- MRI or CT for deeper tissue involvement
Treatment Strategies for Streptococcal Skin and Soft Tissue Infections
Prompt initiation of effective antibiotic therapy and supportive care is critical in managing streptococcal SSSIs.
Recommended Antimicrobial Regimens:
| Infection Type | First-Line Therapy | Alternatives (Penicillin Allergy) |
|---|---|---|
| Impetigo | Oral penicillin, amoxicillin-clavulanate | Cephalexin, clindamycin |
| Erysipelas/Cellulitis | IV penicillin, cefazolin | Clindamycin, vancomycin |
| Necrotizing Fasciitis | IV penicillin + clindamycin | Carbapenems + vancomycin (if polymicrobial) |
| Wound Infections | Targeted therapy post-culture; empirically cover streptococci | Linezolid, doxycycline if MRSA suspected |
Clindamycin is frequently added in severe cases due to its inhibitory effect on toxin production.
Duration:
- Uncomplicated cellulitis: 7–10 days
- Complicated SSSIs or bacteremia: 14–21 days or longer depending on clinical response
Potential Complications from Untreated or Delayed Therapy
Without prompt intervention, streptococcal infections can escalate rapidly and cause systemic involvement.
Serious Complications:
- Sepsis and septic shock
- Acute glomerulonephritis
- Post-streptococcal reactive arthritis
- Endocarditis (in invasive GBS)
- Amputation in necrotizing fasciitis cases
- Chronic wound colonization and reinfection
Preventive Measures for High-Risk Patients
In individuals with recurrent streptococcal skin infections or underlying comorbidities, preventive strategies are essential.
Preventive Approaches:
- Good hygiene and regular skin inspection
- Optimal management of chronic diseases (e.g., diabetes, vascular insufficiency)
- Use of emollients for dry skin conditions
- Prophylactic antibiotics for recurrent cellulitis (e.g., monthly intramuscular benzathine penicillin)
- Compression stockings in venous disease
Differentiating Streptococcal From Other Bacterial SSSIs
Understanding the likely pathogen helps refine antibiotic selection.
| Characteristic | Streptococcus spp. | Staphylococcus aureus |
|---|---|---|
| Lesion margins | Diffuse, indistinct | Localized, well-circumscribed |
| Pus formation | Rare unless mixed infection | Common (abscesses) |
| Toxin-mediated complications | Common (toxic shock, necrosis) | Also possible (especially MRSA) |
| Rapid progression | Yes, especially GAS | Slower compared to GAS infections |
Emerging Therapies and Research Directions
Research continues to evolve in diagnostics, vaccines, and treatment optimization.
- Rapid molecular diagnostics to identify GAS within hours
- Vaccines under development targeting M protein antigens
- Monoclonal antibody therapies under clinical evaluation
- Adjunctive therapies like IVIG in toxic shock syndrome
- Antibiotic stewardship programs to combat resistance
Skin and skin structure infections caused by Streptococcus species require prompt clinical recognition and timely, targeted therapy. With a clear understanding of pathogen-specific features, risk factors, and modern treatment protocols, healthcare providers can significantly reduce the burden of these infections and prevent serious complications. High vigilance, especially in vulnerable populations, remains essential in the ongoing management of streptococcal SSSIs.