Peptostreptococcus is a genus of anaerobic, gram-positive cocci that forms part of the normal microbial flora of the skin, mucous membranes, and gastrointestinal tract. While typically harmless in commensal populations, these bacteria become pathogenic when introduced into sterile tissue via trauma, surgery, or compromised host immunity. Skin and skin structure infections (SSSIs) involving Peptostreptococcus are frequently polymicrobial, co-occurring with other anaerobes and facultative organisms.
Pathogenesis of Peptostreptococcus-Associated SSSIs
Once Peptostreptococcus breaches the skin barrier, it thrives in hypoxic or necrotic tissue environments. Its role in soft tissue infections includes:
- Abscess formation: Driven by the release of destructive enzymes and synergistic interactions with other microbes.
- Chronic infections: Owing to biofilm formation and resistance to host immunity.
- Suppuration and tissue damage: Resulting in significant inflammation and destruction of soft tissue layers.
These infections are typically slow-progressing but can lead to serious complications if left untreated.
Risk Factors for Infection
| Risk Factor | Clinical Relevance |
|---|---|
| Diabetes mellitus | Impairs immune defense and delays wound healing |
| Immunosuppressive therapy | Reduces resistance to opportunistic pathogens |
| Surgical procedures | Breach of sterile tissue introduces anaerobes |
| Pressure ulcers and trauma | Provide anaerobic conditions for bacterial growth |
| Poor hygiene in chronic wounds | Promotes colonization and infection |
Clinical Manifestations of Peptostreptococcus Skin Infections
The signs and symptoms of Peptostreptococcus infections are often nonspecific, requiring high clinical suspicion. Common presentations include:
- Localized cellulitis with erythema, tenderness, and swelling
- Foul-smelling purulent discharge, indicative of anaerobic involvement
- Fluctuant abscesses with systemic signs such as fever and leukocytosis
- Delayed wound healing in post-operative or chronic ulcers
In immunocompromised individuals, dissemination may occur, leading to bacteremia and systemic infection.
Diagnostic Approach to Peptostreptococcal Skin Infections
Clinical Evaluation
- Detailed wound assessment and documentation of odor, exudate, and tissue integrity
- Palpation for fluctuance and signs of necrosis
Laboratory Testing
- Anaerobic culture of aspirated pus or tissue biopsy
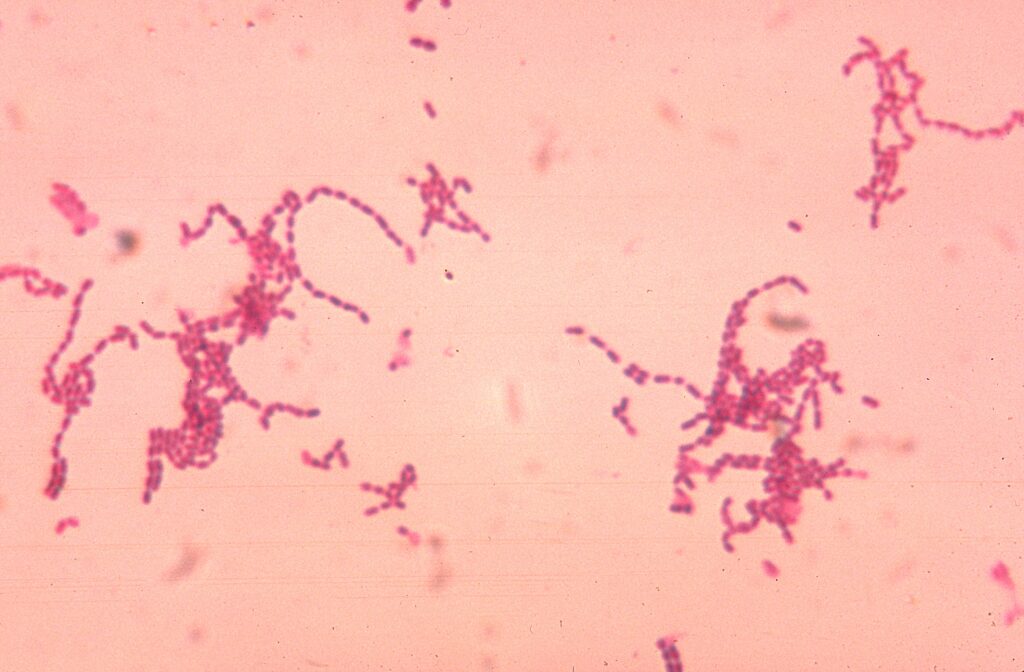
- Gram stain showing gram-positive cocci in chains
- Inflammatory markers: Elevated WBC count, ESR, and CRP
- Blood cultures in cases of systemic symptoms
Imaging Modalities
- Ultrasound or CT scan for detection of deep abscesses
- MRI to assess the extent of soft tissue and fascial involvement
Treatment Guidelines for Peptostreptococcus-Related SSSIs
Empiric Antimicrobial Therapy
Given its anaerobic nature and frequent polymicrobial involvement, therapy must cover both anaerobes and aerobes.
| Severity | First-Line Antibiotics |
|---|---|
| Mild to moderate | Amoxicillin-clavulanate, clindamycin |
| Severe or systemic | Piperacillin-tazobactam, carbapenems (e.g., meropenem) |
| Penicillin allergy | Metronidazole + levofloxacin or clindamycin + ciprofloxacin |
Adjust therapy based on culture sensitivity reports. Duration ranges from 10 to 21 days, depending on infection depth and response.
Surgical and Supportive Management
- Incision and drainage (I&D) for abscesses
- Debridement of necrotic or devitalized tissue
- Negative pressure wound therapy (NPWT) for chronic infections
- Nutritional support and glycemic control in diabetic patients
Complications of Untreated or Improperly Managed Infections
- Chronic fistulae and sinus tract formation
- Spread to deep structures like fascia or bone (osteomyelitis)
- Necrotizing soft tissue infections
- Sepsis or multi-organ dysfunction in severe cases
Early intervention with a combined medical and surgical approach significantly reduces risk of these outcomes.
Prevention and Control Measures
Clinical Practice Recommendations
- Sterile surgical techniques
- Prophylactic antibiotics in high-risk surgeries
- Timely wound care and dressing changes
- Glycemic control in diabetic populations
Outpatient and Community Measures
- Educate patients on signs of infection
- Encourage prompt medical attention for wounds
- Proper management of chronic ulcers or pressure injuries
Skin and skin structure infections due to Peptostreptococcus require a high index of suspicion, especially in anaerobic-prone environments. These infections, while often slow-growing, can result in significant morbidity if not promptly and effectively treated. A multidisciplinary approach involving accurate diagnosis, tailored antibiotic therapy, and appropriate surgical intervention ensures optimal recovery and prevention of recurrence.

