Morganella morganii is a facultative anaerobic, gram-negative bacillus belonging to the Enterobacteriaceae family. Though traditionally considered an opportunistic pathogen, it has emerged as a significant cause of skin and skin structure infections (SSSIs), particularly in immunocompromised individuals, surgical patients, and those with chronic wounds. Its increasing resistance profile adds complexity to clinical management.

Microbiological Characteristics and Pathogenesis
M. morganii exhibits the following virulence and resistance features:
- Urease production, contributing to local tissue alkalinity
- Beta-lactamase activity, enabling resistance to many penicillins
- Biofilm formation, promoting persistence in chronic wounds
- Motility via peritrichous flagella, facilitating tissue invasion
These features allow M. morganii to colonize, evade host defenses, and disseminate within subcutaneous and deep tissue planes.
Common Risk Factors for Morganella morganii SSSIs
- Diabetes mellitus and peripheral neuropathy
- Pressure ulcers and decubitus wounds
- Surgical site infections, particularly abdominal and urological
- Immunosuppression (cancer therapy, organ transplant, HIV)
- Prolonged hospital stays and invasive procedures
- Broad-spectrum antibiotic exposure altering normal flora
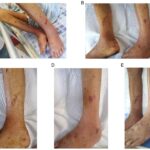
Clinical Manifestations of Morganella Skin and Soft Tissue Infections
Localized Cellulitis
Presents as erythematous, swollen, warm skin with or without purulent discharge. Pain and fever may accompany systemic inflammation.
Abscesses and Wound Infections
Characterized by localized collection of pus, tenderness, fluctuance, and inflammation. Often associated with post-surgical or traumatic wounds.
Necrotizing Fasciitis (Rare)
Aggressive and life-threatening, involving rapid spread along fascial planes. Requires urgent surgical intervention and broad-spectrum antibiotics.
Diagnostic Approach to Morganella morganii SSSI
Clinical Examination
- Assess lesion characteristics: size, depth, warmth, exudate, tenderness
- Evaluate systemic signs: fever, hypotension, leukocytosis
Laboratory and Imaging Workup
- Culture and sensitivity testing from tissue, pus, or wound exudate
- Blood cultures in febrile or septic patients
- Imaging (Ultrasound/CT/MRI) for deep tissue involvement or abscess formation
Antimicrobial Susceptibility Profile and Resistance Concerns
Morganella morganii exhibits intrinsic resistance to:
- Ampicillin and first-generation cephalosporins
- Nitrofurantoin
- Tetracycline (in some strains)
Resistance can be acquired to:
- Fluoroquinolones
- Aminoglycosides
- Carbapenems via ESBL or AmpC production
Regular antimicrobial susceptibility testing is essential for effective treatment selection.
Therapeutic Strategies for Morganella morganii Skin Infections
Empiric Antibiotic Therapy
| Clinical Setting | Empiric Options |
|---|---|
| Community-acquired SSSI | Ceftriaxone, ciprofloxacin |
| Healthcare-associated SSSI | Piperacillin-tazobactam, meropenem |
| Known resistance risk | Carbapenem + aminoglycoside, or colistin if MDR |
Definitive Therapy Based on Culture Results
- Cefepime or fluoroquinolones for susceptible strains
- Carbapenems for ESBL-producing isolates
- Aminoglycosides (gentamicin, amikacin) may be adjuncts
Duration: 7–14 days, adjusted based on clinical resolution and infection severity
Surgical Management and Wound Care
Incision and Drainage
Essential for abscess resolution and reduction of bacterial load.
Debridement
Removal of necrotic or infected tissue, especially in chronic or non-healing wounds.
Wound Healing Optimization
- Use of antimicrobial dressings
- Negative Pressure Wound Therapy (NPWT) for large or slow-healing wounds
- Regular reassessment and dressing change
Potential Complications of Untreated or Improperly Managed Infections
| Complication | Description |
|---|---|
| Bacteremia and Sepsis | Especially in immunocompromised or elderly |
| Chronic Non-Healing Ulcers | Often due to persistent biofilm or poor perfusion |
| Osteomyelitis | Spread to adjacent bone structures |
| Septic Shock | Requires ICU-level care and vasopressors |
| Surgical Intervention Required | In necrotizing infections or abscess recurrence |
Prevention and Infection Control Measures
In Clinical Settings
- Strict aseptic protocols in wound care
- Routine screening and isolation of MDR pathogens
- Rational antibiotic use to limit resistance development
In Community and Long-Term Care
- Optimal glycemic control in diabetics
- Regular inspection and hygiene of wounds or pressure areas
- Early treatment of minor skin lesions to prevent progression
Skin and skin structure infections caused by Morganella morganii are increasingly recognized due to rising antimicrobial resistance and hospital-associated transmission. A multidisciplinary approach involving accurate microbiological diagnosis, resistance-informed antibiotic therapy, timely surgical intervention, and comprehensive wound care ensures optimal outcomes. Vigilant infection control and antimicrobial stewardship remain paramount in preventing nosocomial transmission and preserving therapeutic efficacy.