Klebsiella species, primarily Klebsiella pneumoniae, are gram-negative bacilli associated with healthcare-associated infections and opportunistic community-acquired cases. While most commonly implicated in urinary tract and respiratory infections, Klebsiella can also cause severe skin and skin structure infections (SSSIs), especially in immunocompromised or hospitalized individuals.
Pathogenesis of Klebsiella in Skin and Soft Tissue
Klebsiella species possess virulence factors such as:
- Polysaccharide capsule: Prevents phagocytosis
- Siderophores: Facilitate iron acquisition in host tissues
- Lipopolysaccharides (LPS): Induce inflammatory response
- Biofilm formation: Enhances survival in chronic wounds or devices
These attributes enable Klebsiella to evade host defenses, penetrate compromised skin barriers, and propagate within subcutaneous and muscular tissues.
Risk Factors for Klebsiella SSSIs
- Diabetes mellitus
- Chronic wounds or pressure ulcers
- Peripheral vascular disease
- Immunosuppression (e.g., chemotherapy, HIV)
- Recent surgery or trauma
- Use of invasive medical devices
- Prolonged hospitalization or ICU stay
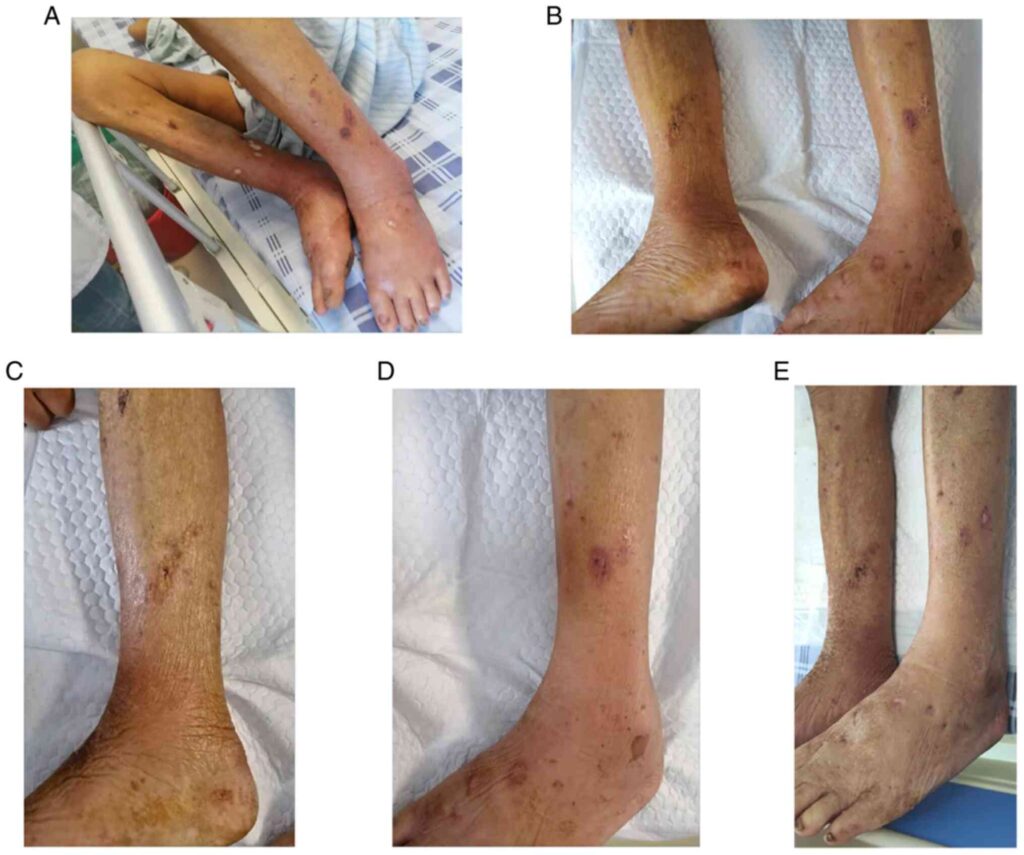
Clinical Presentations of Klebsiella-Related SSSIs
Cellulitis
- Warm, erythematous, and edematous skin
- Painful on palpation
- May progress rapidly, especially in neutropenic patients
Abscess Formation
- Fluctuant, purulent lesions with surrounding induration
- Often requires surgical drainage
Necrotizing Soft Tissue Infection
- Rapid tissue destruction with crepitus and systemic toxicity
- Frequently polymicrobial with Klebsiella as a co-pathogen
Infected Wounds and Surgical Site Infections
- Purulent discharge with delayed wound healing
- May involve biofilm-forming strains resistant to standard treatment
Diagnostic Evaluation
Clinical Examination
- Assess depth, extent, drainage, odor, and tissue necrosis
- Evaluate for signs of systemic infection: fever, leukocytosis, hypotension
Microbiological Testing
- Tissue culture or aspirate is essential for pathogen identification
- Gram stain reveals gram-negative rods
- Sensitivity testing guides appropriate therapy, especially for MDR strains
Imaging
- Ultrasound for abscess delineation
- CT or MRI for deeper infection tracking or necrotizing changes
Antimicrobial Resistance Patterns
Klebsiella species are known for multidrug resistance mechanisms, including:
- Extended-spectrum β-lactamases (ESBLs)
- Carbapenem-resistant Klebsiella pneumoniae (CRKP)
- Plasmid-mediated colistin resistance (mcr genes)
These traits demand precise antimicrobial stewardship and individualized therapy.
Treatment Protocols for Klebsiella Skin and Skin Structure Infections
Empiric Antibiotic Therapy (Pending Culture)
| Risk Level | Recommended Empiric Therapy |
|---|---|
| Community-acquired | Ceftriaxone, ampicillin-sulbactam |
| Hospital-acquired | Piperacillin-tazobactam, cefepime, or meropenem |
| Suspected MDR/CRKP | Ceftazidime-avibactam, meropenem-vaborbactam, colistin |
Targeted Therapy
After culture results, de-escalation to narrow-spectrum antibiotics is advised. Treatment duration typically ranges from 7 to 14 days, depending on clinical response and infection severity.
Surgical and Supportive Management
Drainage and Debridement
- Required for all abscesses and necrotic tissue
- Reduces bacterial load and facilitates antibiotic penetration
Wound Care
- Regular dressing changes
- Use of antimicrobial dressings for persistent colonization
Adjunctive Therapies
- Negative Pressure Wound Therapy (NPWT) for chronic infections
- Hyperbaric Oxygen Therapy (HBOT) in necrotizing infections
Clinical Course and Potential Complications
| Complication | Description |
|---|---|
| Bacteremia | Common in deep or neglected infections |
| Sepsis and Septic Shock | Life-threatening, especially with MDR strains |
| Chronic Wound Infection | Often biofilm-associated and slow to heal |
| Osteomyelitis | May occur with contiguous spread |
| Scarring or Amputation | Especially in necrotizing infections |
Prompt recognition and aggressive treatment can significantly reduce these outcomes.
Infection Control and Prevention
In Healthcare Settings
- Strict hand hygiene and contact precautions
- Isolate patients with known MDR Klebsiella
- Disinfection of reusable medical equipment
In Community Settings
- Wound hygiene and regular dressing
- Early medical attention for infected or non-healing lesions
- Management of comorbidities such as diabetes
Klebsiella skin and skin structure infections, though less common than other bacterial causes, present significant clinical challenges due to their virulence and resistance profiles. A structured approach incorporating early recognition, pathogen-specific therapy, surgical intervention, and stringent infection control is essential. With rising resistance patterns, ongoing surveillance and judicious antibiotic use remain critical to effective management.

