Skin and skin structure infections (SSSIs) encompass a wide spectrum of bacterial infections involving the epidermis, dermis, subcutaneous tissue, fascia, and muscle. These infections vary in severity from mild superficial conditions to life-threatening necrotizing fasciitis. Accurate classification and prompt intervention are vital to minimizing complications and ensuring effective treatment.

Classification of SSSIs Based on Severity and Depth
Uncomplicated SSSIs
- Involve only superficial layers (epidermis and dermis)
- Examples: Impetigo, folliculitis, simple cellulitis
- Typically respond well to oral antibiotics
Complicated SSSIs (cSSSIs)
- Extend to deeper soft tissues or require surgical intervention
- Include abscesses, infected ulcers, burns, and surgical site infections
- Common in immunocompromised patients or those with chronic comorbidities
Acute Bacterial Skin and Skin Structure Infections (ABSSSIs)
Defined by the FDA as:
- Cellulitis/erysipelas
- Wound infections
- Major cutaneous abscesses
Require systemic antimicrobial therapy and often involve pathogens like Staphylococcus aureus and Streptococcus pyogenes.
Common Pathogens in Skin and Skin Structure Infections
| Infection Type | Primary Pathogens |
|---|---|
| Cellulitis/Erysipelas | Streptococcus pyogenes, S. aureus |
| Abscesses | S. aureus (including MRSA) |
| Wound Infections | Polymicrobial including anaerobes, gram-negatives |
| Diabetic Foot Infections | Enterococcus, Pseudomonas, Proteus |
| Necrotizing Infections | Clostridium, Streptococcus, anaerobes |
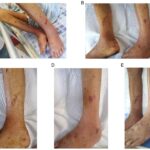
Clinical Manifestations of SSSIs
Cellulitis
- Diffuse, non-purulent inflammation of the dermis and subcutaneous tissue
- Warmth, erythema, tenderness, swelling
- Commonly unilateral in lower extremities
Abscess
- Localized collection of pus
- Fluctuant, tender, with surrounding cellulitis
- Requires incision and drainage
Erysipelas
- Superficial form of cellulitis with raised borders
- Bright red appearance, often involving the face
Wound and Surgical Site Infections
- Develop within 30 days post-procedure (or within 90 days for implants)
- Purulent drainage, localized pain, erythema, and fever
Necrotizing Fasciitis
- Rapidly progressing infection of fascia and soft tissues
- Intense pain, skin discoloration, systemic toxicity
- Requires immediate surgical intervention
Diagnostic Approach to Skin and Skin Structure Infections
Clinical Assessment
- Evaluate extent, location, and progression
- Look for signs of systemic involvement: fever, leukocytosis, hypotension
Microbiological Testing
- Culture of purulent material or tissue
- Blood cultures if systemic signs are present
- Susceptibility testing to guide therapy
Imaging
- Ultrasound for abscess detection
- CT or MRI for deep infections or gas-forming organisms
Treatment Strategies for Skin and Skin Structure Infections
Empiric Antimicrobial Therapy
| Infection Type | Empiric Antibiotics |
|---|---|
| Non-purulent Cellulitis | Penicillin, cephalexin, or clindamycin |
| Purulent Abscess | TMP-SMX, doxycycline, clindamycin (MRSA) |
| Polymicrobial Infections | Ampicillin-sulbactam, piperacillin-tazobactam, carbapenems |
| Necrotizing Infections | Broad-spectrum + clindamycin + surgical debridement |
Targeted Therapy
- Adjust based on culture results
- Narrow-spectrum antibiotics preferred once pathogen identified
Duration of Therapy
- Uncomplicated infections: 5–7 days
- Complicated infections: 10–14 days or more depending on response
Surgical and Adjunctive Interventions
Incision and Drainage (I&D)
- Cornerstone of abscess management
- Antibiotics alone are insufficient
Debridement
- Required for necrotic tissue removal in chronic ulcers or necrotizing infections
Negative Pressure Wound Therapy (NPWT)
- Enhances granulation and healing
- Useful in post-debridement or chronic wounds
Hyperbaric Oxygen Therapy (HBOT)
- Considered in refractory infections, particularly in diabetic foot ulcers or gas gangrene
Risk Factors and Prevention Strategies
Predisposing Conditions
- Diabetes mellitus
- Peripheral vascular disease
- Immunosuppression
- Chronic skin conditions (eczema, psoriasis)
- IV drug use
Preventive Measures
- Good hygiene and skin care
- Timely wound cleaning and dressing
- Prophylactic antibiotics in high-risk surgeries
- Glycemic control in diabetic patients
Complications of Untreated or Severe SSSIs
| Complication | Description |
|---|---|
| Bacteremia | Entry of bacteria into bloodstream |
| Sepsis | Life-threatening systemic inflammation |
| Osteomyelitis | Infection spreads to underlying bone |
| Gangrene | Tissue death requiring amputation |
| Scarring and contractures | Especially post-necrotizing infections |
Prognosis and Outcomes
Timely diagnosis and appropriate therapy result in favorable outcomes in most SSSIs. Delay in treatment, inadequate debridement, or inappropriate antibiotic use increases the risk of morbidity and mortality. Chronic infections may require prolonged therapy and rehabilitation.
Skin and skin structure infections represent a broad clinical challenge that ranges from minor irritation to life-threatening conditions. Effective management relies on rapid identification, pathogen-specific treatment, and when necessary, surgical intervention. A multidisciplinary approach, particularly in complicated or chronic cases, ensures optimal outcomes and minimizes the risk of complications or recurrence.