Citrobacter species, members of the Enterobacteriaceae family, are gram-negative, facultatively anaerobic bacilli. While commonly associated with urinary tract and gastrointestinal infections, they are increasingly implicated in nosocomial skin and skin structure infections (SSSIs), especially in immunocompromised or hospitalized individuals. Among the most clinically relevant are Citrobacter freundii and Citrobacter koseri.
Pathogenesis and Virulence Factors in Citrobacter SSTIs
Citrobacter infections often occur in the context of compromised skin integrity and systemic vulnerability. Key virulence factors include:
- Beta-lactamase production (including AmpC-type enzymes), enabling resistance to many beta-lactam antibiotics
- Adherence mechanisms via pili and surface proteins, facilitating tissue colonization
- Endotoxin production, contributing to inflammation and systemic manifestations
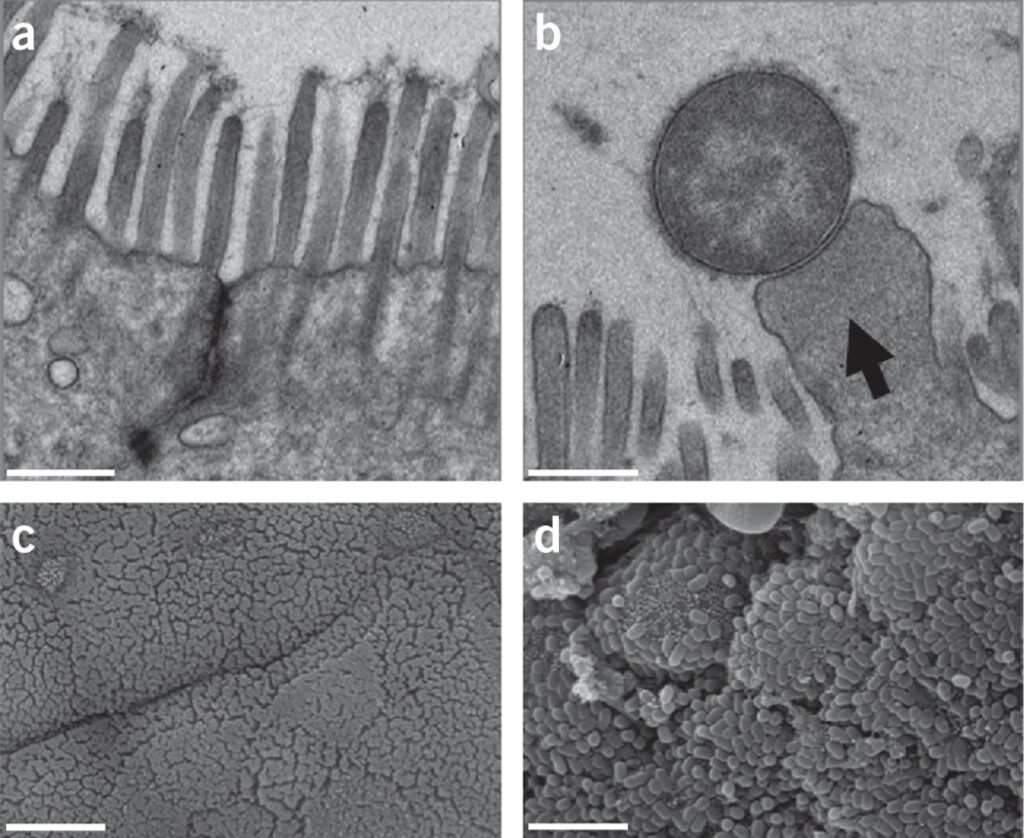
- Biofilm formation on wounds and medical devices, fostering persistence and antimicrobial resistance
These organisms typically gain entry through open wounds, surgical sites, decubitus ulcers, or invasive medical interventions.
Clinical Context and Risk Factors
Skin and skin structure infections due to Citrobacter species are often nosocomial or healthcare-associated. Common predisposing factors include:
- Open surgical wounds or catheter sites
- Burn injuries with prolonged hospital stays
- Chronic ulcers (e.g., diabetic foot ulcers, venous stasis ulcers)
- Pressure sores in bedridden patients
- Long-term corticosteroid use or chemotherapy
- Neonatal intensive care or elderly immunocompromised patients
In these populations, Citrobacter can be isolated either as the primary pathogen or part of a polymicrobial infection.
Characteristic Features of Citrobacter-Induced Skin Infections
Citrobacter SSTIs may range from superficial cellulitis to deep tissue involvement. Typical features include:
- Localized erythema, swelling, and tenderness
- Purulent discharge with a risk of abscess formation
- Systemic signs such as fever and leukocytosis in severe cases
- Delayed wound healing and necrotic tissue in chronic infections
- Rapid progression in immunocompromised hosts or in surgical sites
Diagnostic Approach to Citrobacter Skin and Structure Infections
Laboratory Diagnosis
- Wound Culture and Sensitivity: Essential for pathogen identification and antibiotic susceptibility
- Gram Stain: Shows gram-negative rods, often within neutrophilic infiltrate
- Blood Cultures: Indicated if systemic infection or sepsis is suspected
- Molecular Diagnostics: MALDI-TOF MS and PCR-based methods enhance rapid identification
- Antibiotic Resistance Testing: Crucial due to increasing multidrug-resistant (MDR) Citrobacter strains
Imaging
- Ultrasound or CT Scan: Identifies abscesses or necrotizing soft tissue involvement
- MRI: Useful in evaluating deeper involvement, especially osteomyelitis or myositis
Antibiotic Therapy and Resistance Considerations
Empiric Therapy
Initial empiric therapy should cover gram-negative bacilli, especially in healthcare-associated infections. Agents include:
- Piperacillin-tazobactam
- Cefepime or ceftazidime
- Carbapenems (e.g., meropenem) for ESBL-producing strains
- Fluoroquinolones (e.g., ciprofloxacin) in sensitive isolates
- Aminoglycosides as adjuncts in severe infections
Avoid cephalosporins alone due to potential inducible AmpC resistance.
Definitive Therapy
Tailor based on culture results. Citrobacter spp. often exhibit resistance to:
- Ampicillin
- First- and second-generation cephalosporins
- Clindamycin and macrolides (ineffective against gram-negatives)
Duration depends on infection depth:
- Superficial infections: 7–10 days
- Deep tissue infections: 2–4 weeks with imaging-guided therapy
Surgical and Supportive Management
- Drainage of abscesses when present
- Debridement of necrotic or infected tissue
- Wound care optimization with antiseptic dressings
- Negative-pressure wound therapy (NPWT) in chronic or non-healing ulcers
- Nutritional support and glycemic control to promote healing
Early surgical intervention and wound source control are essential to reduce bacterial burden and hasten recovery.
Multidrug Resistance in Citrobacter Species
Resistance mechanisms in Citrobacter include:
- AmpC beta-lactamases, often chromosomally encoded
- Extended-spectrum beta-lactamases (ESBLs) in nosocomial isolates
- Carbapenem resistance via porin loss or efflux pumps
- Plasmid-mediated resistance enabling horizontal gene transfer
These traits demand careful antibiotic stewardship and isolation precautions in hospital settings.
Clinical Outcomes and Prognosis
The prognosis of Citrobacter SSTIs depends on:
- Host immunity and comorbidities
- Timeliness of diagnosis and intervention
- Presence of MDR organisms
- Extent of tissue involvement
With prompt, targeted therapy and appropriate wound management, outcomes are generally favorable. However, delays may lead to systemic dissemination, requiring intensive care.
Prevention of Citrobacter Skin Infections in Clinical Settings
- Strict hand hygiene and aseptic protocols in healthcare environments
- Sterile dressing changes and catheter care
- Routine wound surveillance in high-risk patients
- Minimization of unnecessary catheter use
- Antibiotic stewardship to reduce selection pressure for resistance
Citrobacter species, though not the most common skin pathogens, pose significant challenges in healthcare-associated skin and soft tissue infections due to their multidrug resistance and opportunistic nature. Accurate diagnosis, prompt empiric treatment, surgical intervention when necessary, and guided antimicrobial therapy are essential to ensure optimal patient outcomes. Vigilance in hospital environments, especially in vulnerable populations, remains critical to mitigating infection risks and controlling spread.

