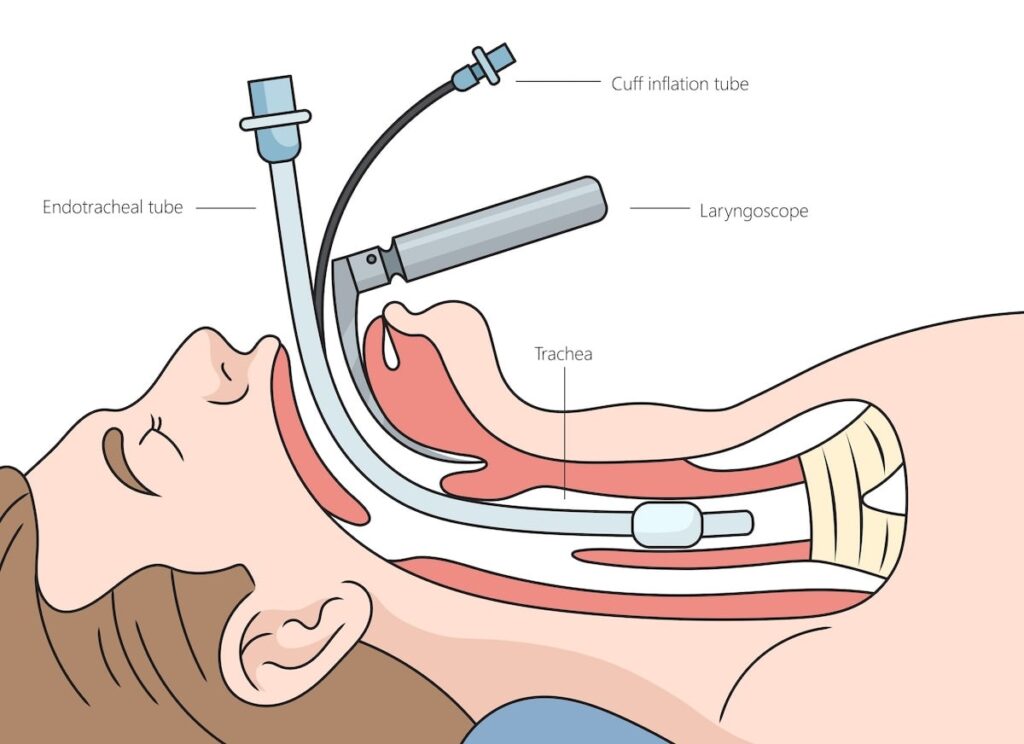
Endotracheal intubation is a critical procedure in airway management requiring adequate suppression of airway reflexes and muscular activity. Skeletal muscle relaxation facilitates this by allowing optimal laryngoscopic view, minimizing trauma, and preventing patient movement. The use of neuromuscular blocking agents (NMBAs) during rapid sequence induction (RSI) or elective intubation is standard practice to achieve profound muscle paralysis for swift and safe intubation.
Mechanism of Action: Neuromuscular Blockers in Intubation
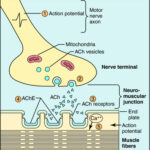
Neuromuscular blockers work at the neuromuscular junction by inhibiting acetylcholine transmission, resulting in skeletal muscle paralysis. They are categorized into two classes based on their mode of receptor interaction:
Depolarizing Neuromuscular Blockers
- Example: Succinylcholine
- Mechanism: Mimics acetylcholine, binds to nicotinic receptors, causing continuous depolarization and transient fasciculations followed by flaccid paralysis.
- Onset/Duration: Rapid onset (<60 seconds); short duration (5–10 minutes)
Non-Depolarizing Neuromuscular Blockers
- Examples: Rocuronium, Vecuronium, Cisatracurium
- Mechanism: Competitively inhibit acetylcholine without causing depolarization.
- Onset/Duration: Varies by agent; Rocuronium offers a rapid onset alternative to succinylcholine.
Indications for Muscle Relaxation During Intubation
- Facilitation of laryngoscopy and tracheal tube placement
- Prevention of laryngospasm and coughing
- Reduction of intracranial and intraocular pressure fluctuations
- Muscle tone suppression for safe airway device passage
- Improved intubation conditions in RSI or controlled settings
Drug Selection: Choosing the Optimal Muscle Relaxant
Selection depends on urgency, patient-specific factors (e.g., renal/hepatic function), and procedure duration. Below is a comparison of commonly used agents.
| Agent | Type | Onset (sec) | Duration (min) | Reversal | Key Features |
|---|---|---|---|---|---|
| Succinylcholine | Depolarizing | 30–60 | 5–10 | Spontaneous hydrolysis | Fastest onset, contraindicated in hyperkalemia |
| Rocuronium | Non-depolarizing | 60–90 | 30–60 | Sugammadex | Alternative to succinylcholine |
| Vecuronium | Non-depolarizing | 120–180 | 45–60 | Neostigmine or Sugammadex | Intermediate duration |
| Cisatracurium | Non-depolarizing | 120 | 30–60 | Spontaneous degradation (Hofmann elimination) | Ideal in organ dysfunction |
Rapid Sequence Induction (RSI) and Muscle Relaxants
RSI is the preferred technique in emergency intubation where aspiration risk is high. Muscle relaxants used in RSI must provide quick and profound paralysis.
Standard RSI Protocol:
- Preoxygenation (3–5 minutes)
- Induction agent (e.g., Etomidate, Propofol, Ketamine)
- Immediate NMBA administration (e.g., Succinylcholine or Rocuronium)
- No ventilation until after intubation
- Confirm endotracheal tube placement
Special Populations and Contraindications
Succinylcholine Contraindications:
- Hyperkalemia (burns, trauma, renal failure)
- Malignant hyperthermia susceptibility
- Neuromuscular disorders (e.g., ALS, Guillain-Barré)
- Denervation injuries
- Pseudocholinesterase deficiency
Preferred Agents in Special Cases:
- Rocuronium in contraindication to Succinylcholine
- Cisatracurium in renal or hepatic dysfunction
- Sugammadex for rapid reversal of aminosteroid NMBAs
Reversal of Neuromuscular Blockade
Timely and complete reversal of non-depolarizing NMBAs is essential to avoid residual paralysis post-extubation.
Reversal Agents:
- Neostigmine: Acetylcholinesterase inhibitor; requires antimuscarinic (e.g., Glycopyrrolate) co-administration.
- Sugammadex: Selective binding agent for Rocuronium and Vecuronium; enables rapid and complete reversal.
Monitoring Neuromuscular Blockade
Objective neuromuscular monitoring (quantitative Train-of-Four monitoring) is crucial to:
- Assess depth of blockade
- Guide timing of intubation
- Confirm recovery before extubation
Train-of-Four (TOF):
- Electrical stimulation of a peripheral nerve
- Evaluation of muscle twitch response
- 0/4 twitches = full blockade; ≥4/4 = adequate recovery
Safety Considerations and Adverse Effects
While muscle relaxants enhance intubation safety, potential complications exist.
Succinylcholine Risks:
- Bradycardia
- Hyperkalemia-induced arrhythmia
- Malignant hyperthermia
- Increased intracranial/intraocular/intragastric pressure
Non-Depolarizing Agent Risks:
- Prolonged paralysis
- Hypersensitivity reactions
- Incomplete reversal leading to postoperative respiratory depression
Clinical Best Practices
- Always verify NMBA indications and contraindications.
- Monitor neuromuscular function throughout the procedure.
- Choose agents based on patient comorbidities and context.
- Ensure appropriate reversal and extubation criteria before awakening.
- Be prepared to manage airway complications, especially in emergency RSI.
Skeletal muscle relaxation is a cornerstone of effective and safe endotracheal intubation. A precise understanding of the pharmacology, selection criteria, and patient-specific considerations of neuromuscular blockers ensures optimal intubation conditions and minimizes complications. Clinicians must tailor agent choice and monitoring strategies to each clinical scenario to ensure the highest standards in airway management.