Sjogren’s syndrome is a chronic systemic autoimmune disorder that primarily targets the body’s exocrine glands—most notably the salivary and lacrimal glands—leading to dryness of the mouth and eyes. It can occur as a primary condition or in conjunction with other autoimmune diseases such as rheumatoid arthritis or lupus. Though often underdiagnosed due to its slow onset and overlapping symptoms, Sjogren’s syndrome affects millions globally, particularly middle-aged women.
Causes and Pathophysiology of Sjogren’s Syndrome
Sjogren’s syndrome arises from a dysregulated immune response where lymphocytes infiltrate and damage the exocrine glands. The condition is idiopathic but believed to result from a complex interplay of genetic predisposition, environmental triggers (such as viral infections), and hormonal factors. Human leukocyte antigen (HLA) gene variants, particularly HLA-DR and HLA-DQ, have been implicated in increasing susceptibility.
The immune system inappropriately targets and destroys moisture-producing glands, impairing their function and triggering systemic inflammation that can affect organs including the lungs, kidneys, liver, and nervous system.
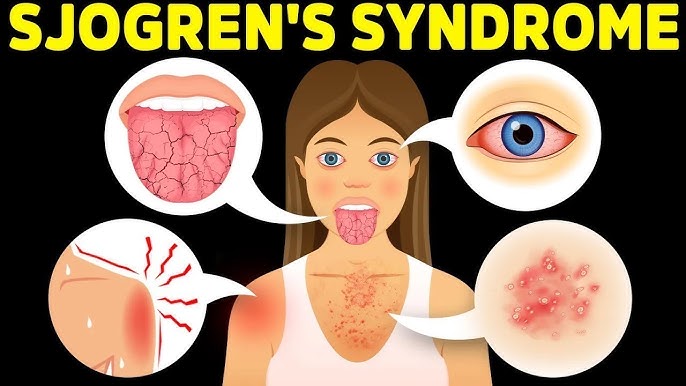
Common Signs and Symptoms of Sjogren’s Syndrome
The hallmark symptoms of Sjogren’s syndrome are xerostomia (dry mouth) and keratoconjunctivitis sicca (dry eyes). However, systemic involvement extends far beyond the exocrine glands.
Primary Symptoms:
- Dry Mouth (Xerostomia): Difficulty swallowing, speaking, or tasting; increased dental decay.
- Dry Eyes (Keratoconjunctivitis Sicca): Burning, itching, or a gritty sensation in the eyes.
Secondary Symptoms:
- Parotid gland enlargement
- Fatigue and malaise
- Joint pain or stiffness
- Vaginal dryness
- Dry skin and nasal passages
Systemic Involvement:
- Pulmonary: Interstitial lung disease, chronic cough
- Renal: Tubulointerstitial nephritis
- Neurological: Peripheral neuropathy, cognitive dysfunction
- Hematological: Lymphoma (non-Hodgkin’s type in severe cases)
Diagnostic Criteria for Sjogren’s Syndrome
Diagnosis is complex due to the variability of symptoms and overlap with other autoimmune diseases. It typically involves clinical evaluation, laboratory tests, and tissue biopsy.
Diagnostic Components:
- Schirmer’s Test: Measures tear production.
- Sialometry: Measures saliva output.
- Autoantibody Testing:
- Anti-SSA (Ro) and Anti-SSB (La) antibodies
- Rheumatoid factor (RF) and antinuclear antibodies (ANA)
- Labial Salivary Gland Biopsy: Identifies lymphocytic infiltration (focus score ≥1).
- Ocular Staining Score: Evaluates damage to the surface of the eye.
Classification: Primary vs. Secondary Sjogren’s Syndrome
- Primary Sjogren’s Syndrome: Occurs in isolation without other autoimmune conditions.
- Secondary Sjogren’s Syndrome: Accompanies autoimmune diseases such as:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Scleroderma
- Polymyositis
Understanding this classification is vital for treatment planning and monitoring for systemic complications.
Complications Associated with Sjogren’s Syndrome
If left untreated or poorly managed, Sjogren’s syndrome can lead to severe complications, including:
- Dental Caries and Oral Infections: Resulting from reduced saliva production.
- Corneal Ulcers and Eye Infections: Due to insufficient tear production.
- Lymphoma: Increased risk, especially MALT lymphoma in salivary glands.
- Interstitial Lung Disease: Can impair respiratory function.
- Kidney Involvement: May lead to renal tubular acidosis.
Treatment Options for Sjogren’s Syndrome
While there is no definitive cure for Sjogren’s syndrome, targeted treatments help alleviate symptoms and minimize systemic complications.
Symptomatic Treatment:
- Artificial Tears and Eye Lubricants
- Saliva Substitutes and Stimulants
- Pilocarpine and Cevimeline (muscarinic agonists)
- Dental Hygiene Products
- Fluoride rinses and regular dental care
Systemic Therapies:
- Hydroxychloroquine: Effective in treating joint and fatigue symptoms.
- Corticosteroids and Immunosuppressants:
- Methotrexate, azathioprine for severe organ involvement.
- Biologics:
- Rituximab (anti-CD20 monoclonal antibody) used in refractory cases or lymphoma risk.
Lifestyle Adjustments:
- Hydration and Humidifiers: Prevents dryness in eyes, mouth, and skin.
- Smoking Cessation: Tobacco worsens dryness symptoms.
- Regular Exercise and Stress Reduction: Improves fatigue and general well-being.
Prognosis and Long-Term Management
Sjogren’s syndrome is generally manageable but requires ongoing surveillance. Patients with glandular-only involvement typically have a good prognosis. However, systemic involvement increases the risk of morbidity. Regular screening for lymphoma and organ function assessment is critical for long-term care.
Prognostic factors include:
- Age at diagnosis
- Degree of systemic involvement
- Presence of SSA/SSB antibodies
- Development of cryoglobulinemia or vasculitis
Sjogren’s syndrome is a multifaceted autoimmune disorder that impacts both glandular and systemic health. Early recognition, accurate diagnosis, and tailored treatment are crucial to improving quality of life and preventing serious complications. Through vigilant management and multidisciplinary care, patients can achieve symptom control and maintain functional health.

