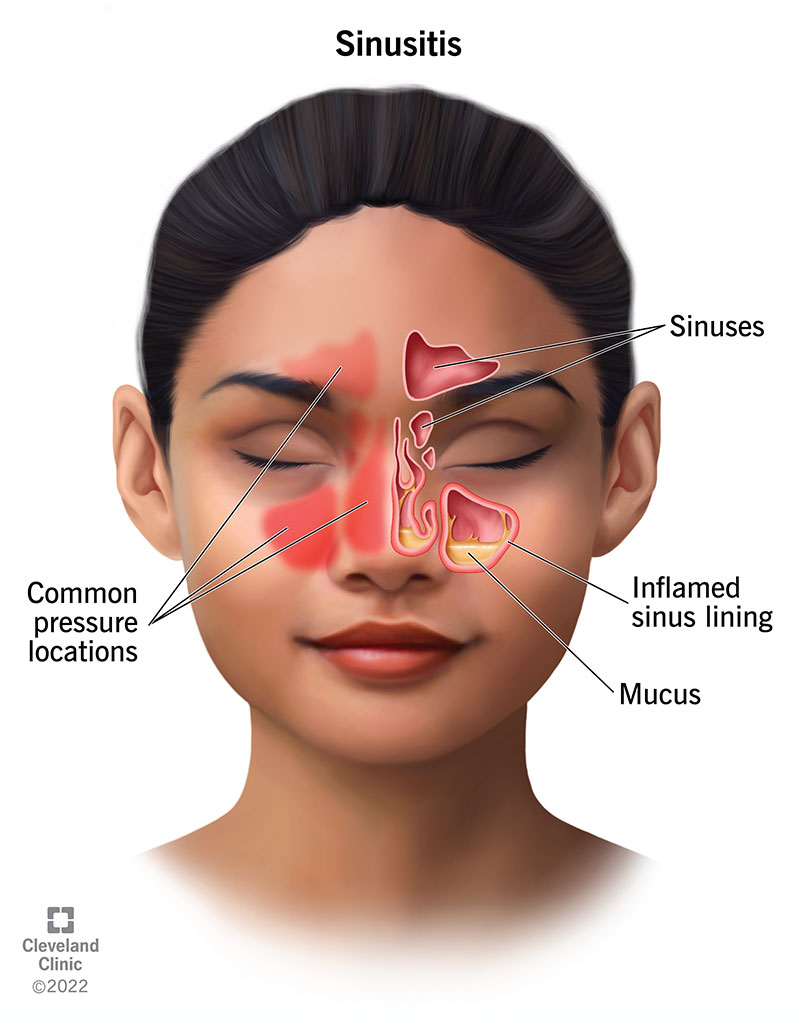
Sinusitis, also known as rhinosinusitis, refers to inflammation of the mucosal lining of the paranasal sinuses. It is a common clinical condition affecting millions globally, contributing to significant healthcare burden and diminished quality of life. Sinusitis may be acute or chronic, with etiologies ranging from infectious to structural or allergic triggers.
Types of Sinusitis: Acute vs. Chronic
Acute Sinusitis
- Duration: Typically less than 4 weeks
- Etiology: Viral upper respiratory infections are the most frequent cause, though bacterial superinfection may occur.
- Symptoms: Sudden onset of facial pain, nasal congestion, purulent nasal discharge, fever, and reduced sense of smell.
Chronic Sinusitis
- Duration: Persists beyond 12 weeks
- Etiology: Often multifactorial—includes persistent infections, allergies, nasal polyps, or anatomical obstructions.
- Symptoms: Nasal obstruction, postnasal drip, chronic cough, facial pressure, fatigue, and anosmia.
Anatomical Overview of the Paranasal Sinuses
Each sinus is lined with mucosa and drains into the nasal cavity. Obstruction of these pathways leads to mucus retention, infection, and inflammation.
Primary Causes of Sinusitis
- Infections: Viral (e.g., rhinovirus), bacterial (e.g., Streptococcus pneumoniae), and rarely fungal (in immunocompromised hosts).
- Allergies: Allergic rhinitis may lead to chronic inflammation and mucosal swelling.
- Structural Abnormalities: Deviated septum, nasal polyps, or concha bullosa can impede sinus drainage.
- Environmental Factors: Pollution, tobacco smoke, and changes in air pressure.
- Immune Deficiencies: Recurrent or chronic infections may signal underlying immunodeficiency.
Common Signs and Symptoms of Sinusitis
| Symptom | Description |
|---|---|
| Facial Pain/Pressure | Especially over sinuses (forehead, cheeks) |
| Nasal Congestion | Difficulty breathing through the nose |
| Purulent Nasal Discharge | Thick yellow or green mucus |
| Headache | Often worse when bending forward |
| Postnasal Drip | Mucus drainage into the throat |
| Tooth Pain | Particularly upper molars |
| Cough | Especially at night, due to mucus drainage |
| Fever | More common in bacterial sinusitis |
Diagnostic Approaches for Sinusitis
Clinical Evaluation
Diagnosis is primarily clinical, based on history and physical examination. Key indicators include:
- Duration of symptoms
- Nature of nasal discharge
- Presence of fever or facial tenderness
- Endoscopic nasal examination for persistent cases
Imaging Studies
- CT Scan of the Sinuses: Gold standard for evaluating chronic or complicated cases.
- MRI: Useful in distinguishing fungal or neoplastic processes.
- Nasal Endoscopy: Enables direct visualization of sinus openings and mucosal pathology.
Treatment Options for Sinusitis
Acute Sinusitis Management
Viral Sinusitis
- Supportive care: saline nasal irrigation, steam inhalation, rest
- Analgesics: ibuprofen or acetaminophen
- Nasal decongestants (short-term): oxymetazoline (limit to 3 days)
Bacterial Sinusitis
- Indications for antibiotics:
- Persistent symptoms >10 days
- Severe symptoms including high fever
- Worsening after initial improvement
- First-line therapy: Amoxicillin-clavulanate
- Alternatives: doxycycline or respiratory fluoroquinolones (if allergic to penicillin)
Chronic Sinusitis Treatment
- Intranasal corticosteroids: Fluticasone, mometasone
- Saline irrigations: Daily use to improve mucociliary clearance
- Antibiotics: Based on culture, often 3–6 weeks of treatment
- Leukotriene modifiers: For patients with coexisting allergies
- Surgery (Functional Endoscopic Sinus Surgery – FESS): For anatomical obstructions or refractory cases
Sinusitis in Special Populations
Children
- More likely to present with cough, irritability, and nasal congestion
- Avoid prolonged use of over-the-counter decongestants
Immunocompromised Individuals
- Increased risk of invasive fungal sinusitis (e.g., mucormycosis)
- Require immediate imaging and possible surgical debridement
Pregnant Women
- Use non-pharmacologic options primarily
- Consult physician before using any medications
Preventive Strategies for Sinusitis
- Avoid allergens and irritants
- Use humidifiers to maintain nasal moisture
- Practice regular nasal saline irrigation
- Manage allergic rhinitis aggressively
- Address underlying structural abnormalities promptly
Complications of Untreated or Recurrent Sinusitis
- Orbital cellulitis or abscess
- Osteomyelitis of the facial bones
- Meningitis
- Cavernous sinus thrombosis
- Chronic mucosal remodeling
Prompt diagnosis and adherence to treatment protocols are crucial in preventing such sequelae.
Sinusitis is a prevalent yet manageable condition when addressed with a thorough understanding of its underlying causes, accurate diagnosis, and structured treatment approach. From acute viral forms to complex chronic cases, comprehensive care incorporating medical, surgical, and preventive strategies ensures symptom resolution and enhanced quality of life.