Sinus tachycardia secondary to antipsychotic medication is a clinically significant yet under-recognized cardiovascular side effect encountered in psychiatric treatment. The interplay between neuroleptic drugs and cardiac conduction systems requires thorough understanding to ensure safe psychopharmacologic practice. Recognizing this adverse effect is vital in preventing misdiagnosis, optimizing therapy, and reducing cardiovascular risk.
Pathophysiology: How Antipsychotics Induce Sinus Tachycardia
Antipsychotic medications, both typical and atypical, can alter autonomic tone and impact cardiac electrophysiology. The mechanism of sinus tachycardia in these cases is multifactorial:
- Anticholinergic activity: Drugs like clozapine and olanzapine inhibit parasympathetic control, leading to unopposed sympathetic stimulation.
- Alpha-1 adrenergic blockade: Results in peripheral vasodilation and reflex tachycardia.
- Direct stimulation of β-adrenergic receptors: Enhances SA node activity.
- QT prolongation and cardiac repolarization abnormalities: Though more associated with arrhythmias, these changes may indirectly influence sinus rate.
Common Antipsychotics Associated with Sinus Tachycardia
| Drug | Tachycardia Risk | Mechanism |
|---|---|---|
| Clozapine | High | Strong anticholinergic + alpha-1 blockade |
| Olanzapine | Moderate | Anticholinergic effect |
| Quetiapine | Moderate | Mild anticholinergic effect |
| Risperidone | Low–Moderate | Minimal autonomic effects |
| Haloperidol | Low | Rare; possible with IV use |
| Ziprasidone | Low | More associated with QT prolongation |
Clinical Presentation
Sinus tachycardia secondary to antipsychotic drugs may present with:
- Resting heart rate >100 bpm
- Palpitations
- Dizziness or lightheadedness
- Mild chest discomfort
- Exacerbation of anxiety symptoms
- In severe cases, progression to arrhythmias in vulnerable patients
This tachycardia typically emerges within days to weeks of drug initiation or dose escalation, particularly in rapid titration scenarios.
ECG Characteristics in Drug-Induced Sinus Tachycardia
- Heart Rate: >100 bpm, typically 100–140 bpm
- P Wave: Upright in leads I and II, preceding every QRS
- PR Interval: Normal
- QRS Duration: Normal
- QT Interval: May be prolonged in some agents, such as clozapine or ziprasidone
Diagnostic Considerations
Key Evaluation Steps
- Detailed Medication History: Note recent additions, dose changes, or polypharmacy.
- Vital Signs and Physical Exam: Rule out fever, dehydration, or other confounders.
- Electrocardiogram: Confirm sinus origin and rule out atrial or ventricular arrhythmias.
- Laboratory Tests:
- CBC (infection/anemia)
- Thyroid panel (thyrotoxicosis)
- Electrolytes (especially potassium and magnesium)
Differential Diagnosis
| Differential | Key Feature |
|---|---|
| Anxiety/Panic | Episodic, with hyperventilation |
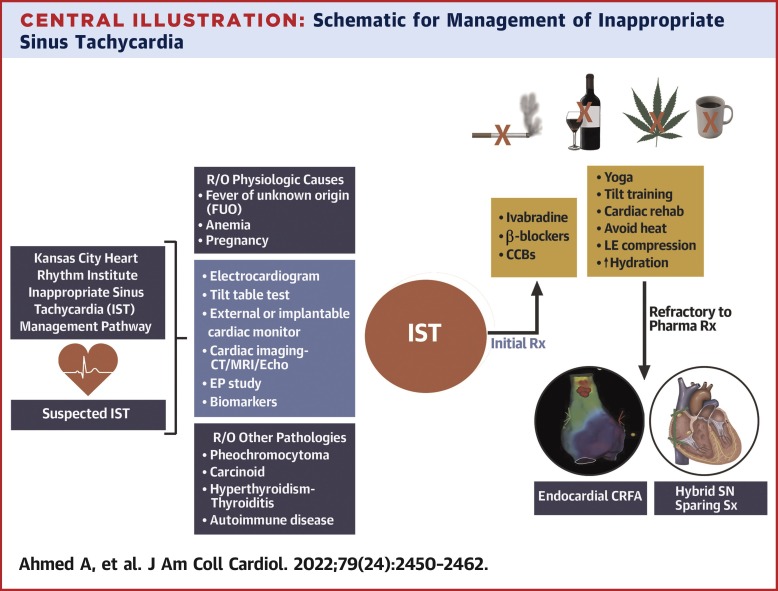
| Inappropriate Sinus Tachycardia | No clear trigger, persistent |
| Hyperthyroidism | Weight loss, tremor, heat intolerance |
| Supraventricular Tachycardia | Abrupt onset, no visible P waves |
| Dehydration | Hypotension, dry mucosa |
Management Strategies
Immediate Approach
- Discontinue or reduce offending agent when clinically feasible.
- Evaluate for alternative medications with fewer cardiac side effects.
- Symptomatic relief may be provided using cardioselective beta-blockers (e.g., metoprolol) if no contraindications exist.
Pharmacologic Options
| Drug | Use | Precautions |
|---|---|---|
| Metoprolol | Symptom control | Avoid in severe asthma or bradycardia |
| Ivabradine | Off-label; selective SA node inhibition | Cost, limited psychiatric data |
| Diltiazem | Alternative to β-blockers | Watch for bradycardia in polytherapy |
Non-Pharmacologic Measures
- Gradual titration of antipsychotics
- Avoid co-administration with stimulants
- Monitor ECG and vitals during dose adjustments
- Encourage hydration and stress reduction
Special Considerations for Clozapine-Induced Tachycardia
Clozapine is highly effective but notorious for causing sinus tachycardia. Persistent heart rate elevations >120 bpm may signal myocarditis, a rare but serious complication requiring urgent cessation and cardiologic evaluation. Regular monitoring during initiation and titration is mandatory.
Prognosis and Monitoring
In most cases, sinus tachycardia secondary to antipsychotics resolves with dose reduction, discontinuation, or supportive therapy. However, continuous ECG surveillance and cardiovascular assessment are recommended, especially in patients with preexisting cardiac disease or high cumulative antipsychotic doses.
Sinus tachycardia secondary to antipsychotic medication represents a pharmacologic side effect with important diagnostic and therapeutic implications. Timely recognition, risk stratification, and collaborative management between psychiatry and cardiology are key to ensuring optimal outcomes. Tailoring antipsychotic use based on individual cardiovascular risk can significantly enhance patient safety in long-term psychiatric care.

