Sinus tachycardia is a condition where the sinoatrial (SA) node increases its firing rate, resulting in a heart rate exceeding 100 beats per minute while maintaining a normal rhythm. This physiological or pathological elevation in heart rate may be transient or persistent, depending on the underlying cause. Proper evaluation is essential to distinguish between appropriate and inappropriate sinus tachycardia and to guide effective management.
Physiology of the Sinoatrial Node and Heart Rate Regulation
The sinoatrial node, located in the right atrium near the superior vena cava, serves as the primary pacemaker of the heart. It generates impulses that travel through the atria, AV node, bundle branches, and Purkinje fibers, ensuring coordinated contraction.
Heart rate is influenced by autonomic input, circulating catecholamines, metabolic demands, and systemic conditions. Sinus tachycardia reflects increased sympathetic or reduced parasympathetic activity.
Clinical Features of Sinus Tachycardia
Common Symptoms
- Palpitations
- Lightheadedness
- Fatigue
- Dyspnea
- Chest discomfort
- Anxiety (in inappropriate cases)
In many instances, sinus tachycardia is asymptomatic and incidentally discovered during routine ECG or physical examination.
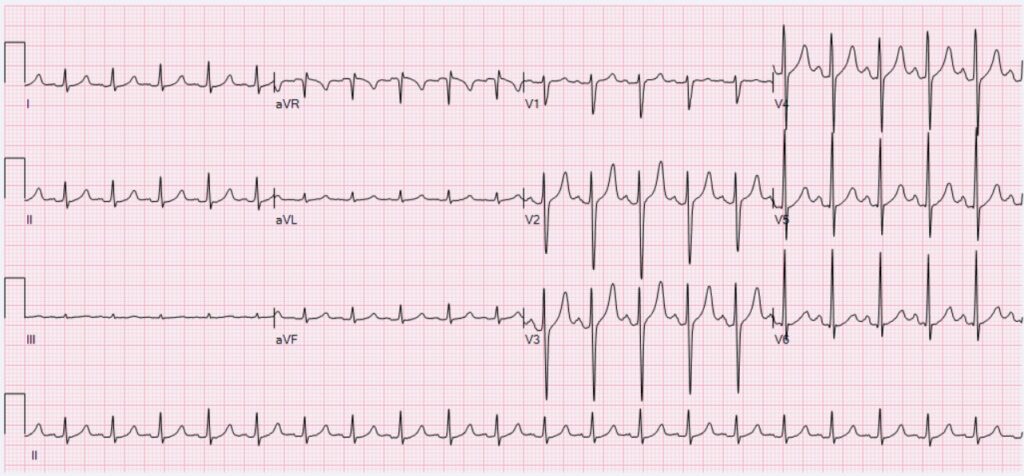
ECG Characteristics of Sinus Tachycardia
- Heart rate: >100 bpm (typically up to 150–180 bpm in physiological states)
- Rhythm: Regular
- P waves: Upright in leads I and II, preceding each QRS
- PR interval: Normal
- QRS complex: Narrow (<120 ms)
- QT interval: Shortens as heart rate increases
These features distinguish sinus tachycardia from atrial tachyarrhythmias and supraventricular tachycardia.
Differentiating Physiological and Inappropriate Sinus Tachycardia
Physiological Sinus Tachycardia (Appropriate)
Occurs as a compensatory response to stimuli:
- Fever
- Exercise
- Pain
- Hypovolemia
- Anemia
- Hypoxia
- Thyrotoxicosis
- Sepsis
- Heart failure
- Drug effects (e.g., stimulants, beta-agonists)
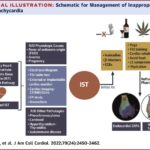
Inappropriate Sinus Tachycardia (IST)
- Resting heart rate >100 bpm or exaggerated response to minimal exertion
- No identifiable physiological trigger
- Often associated with autonomic dysfunction or hypersensitivity of the SA node
IST is a diagnosis of exclusion and typically affects young, otherwise healthy individuals.
Causes of Sinus Tachycardia
| Cause Category | Examples |
|---|---|
| Physiological | Exercise, anxiety, pain |
| Hypovolemia | Hemorrhage, dehydration |
| Endocrine | Hyperthyroidism, pheochromocytoma |
| Infectious | Sepsis, fever, systemic inflammation |
| Pulmonary | Hypoxia, pulmonary embolism |
| Cardiac | Heart failure, pericarditis |
| Pharmacologic | Caffeine, nicotine, sympathomimetics |
| Toxicologic | Withdrawal syndromes, illicit drugs |
Diagnostic Approach
History and Physical Examination
A detailed clinical history is vital to identify triggers, medication use, and systemic symptoms.
Laboratory Tests
- CBC (to rule out anemia or infection)
- TSH, T3, T4 (thyroid function)
- Electrolyte panel
- Cardiac biomarkers (if myocardial ischemia suspected)
Electrocardiogram (ECG)
Essential to confirm sinus origin and exclude atrial or ventricular arrhythmias.
Additional Tests
- Echocardiogram (to assess structural heart disease)
- Holter monitoring (to evaluate persistent tachycardia or variability)
- Tilt-table testing (for autonomic dysfunction in IST)
Management of Sinus Tachycardia
Treat Underlying Cause
In physiological cases, resolution is typically achieved by addressing the precipitating factor:
- Rehydration for hypovolemia
- Antipyretics for fever
- Beta-blockers for thyrotoxicosis
- Oxygen therapy for hypoxia
Pharmacological Therapy
Reserved for symptomatic or persistent cases not due to reversible causes.
Beta-Blockers
- Metoprolol, atenolol
- First-line for inappropriate sinus tachycardia or anxiety-related tachycardia
Calcium Channel Blockers
- Verapamil or diltiazem may be considered in selected patients
Ivabradine
- Selectively inhibits the If current in the SA node
- Useful in IST unresponsive to conventional therapy
Non-Pharmacologic Interventions
- Vagal maneuvers (in acute episodes)
- Avoidance of triggers (caffeine, stress)
- Lifestyle modifications (hydration, sleep hygiene)
Ablation Therapy
Radiofrequency catheter ablation may be considered in refractory IST, though risk to the SA node remains a concern.
Prognosis and Long-Term Outlook
Physiological sinus tachycardia generally resolves with appropriate treatment of the underlying cause. Inappropriate sinus tachycardia, although benign, may significantly impair quality of life due to persistent symptoms. With proper diagnosis and individualized therapy, most patients experience substantial improvement.
Sinus tachycardia is a common cardiac rhythm characterized by an elevated but organized heart rate originating from the sinoatrial node. It may be a benign physiological response or part of a more complex syndrome such as inappropriate sinus tachycardia. Accurate diagnosis, identification of reversible causes, and symptom-guided management remain the pillars of effective care.