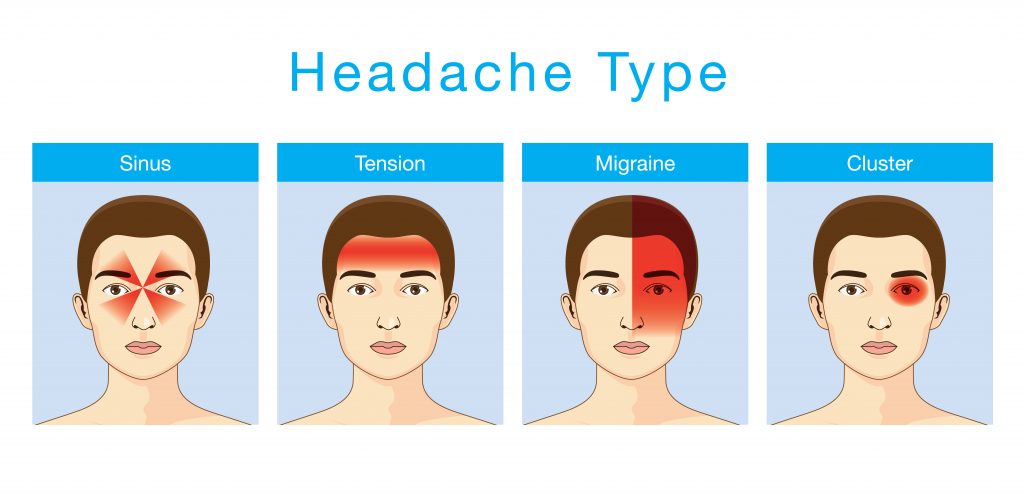
Sinus headache is characterized by pain and pressure in the face due to inflammation or infection of the paranasal sinuses. While commonly attributed to sinusitis, many cases initially diagnosed as sinus headaches may actually stem from migraines or other primary headache disorders. Accurate identification and targeted management are essential for long-term relief.
Anatomy of the Sinuses and Headache Origin
The human skull contains four pairs of sinuses—frontal, maxillary, ethmoidal, and sphenoidal. These air-filled cavities are lined with mucosa and drain into the nasal passages.
When the drainage is obstructed due to infection, inflammation, or allergies, pressure builds, leading to facial pain and discomfort commonly referred to as a sinus headache.
Key Symptoms of Sinus Headache
True sinus headaches typically present with the following features:
- Deep, dull, or throbbing pain in the forehead, cheeks, or around the eyes
- Worsening pain with head movement or straining
- Nasal congestion or discharge
- Tenderness over the sinus areas
- Facial swelling or fullness
- Reduced sense of smell
Symptoms often coincide with or follow upper respiratory tract infections or allergic rhinitis. The presence of fever, purulent nasal discharge, and fatigue can indicate sinusitis.
Sinus Headache vs. Migraine: Critical Differences
A high proportion of self-reported sinus headaches are actually migraines. Differentiation is key to appropriate treatment.
| Feature | Sinus Headache | Migraine |
|---|---|---|
| Pain Location | Forehead, cheeks, nasal bridge | One-sided, can shift |
| Onset | With or after cold/allergies | Gradual, without infection |
| Nasal Symptoms | Present (congestion, discharge) | Rare |
| Associated Symptoms | Fever, facial tenderness | Nausea, photophobia, aura |
| Response to Decongestants | Often effective | Minimal |
Clinicians must exercise caution to avoid misdiagnosis and consequent mistreatment.
Common Causes of Sinus Headache
Infections
- Acute bacterial sinusitis
- Viral upper respiratory infections
- Fungal sinus infections (rare)
Allergic Reactions
- Allergic rhinitis causing mucosal swelling and impaired drainage
Anatomical Blockages
- Deviated nasal septum
- Nasal polyps
- Turbinate hypertrophy
Environmental Triggers
- Pollution
- Cold or dry air
- Occupational irritants
Diagnostic Approach to Sinus Headache
Clinical Examination
- Palpation and percussion of sinus areas
- Anterior rhinoscopy for mucosal swelling or discharge
Imaging Studies
- CT Scan of the sinuses: Gold standard for confirming sinusitis
- MRI: Used when neoplastic or fungal etiology is suspected
Endoscopic Evaluation
- Nasal endoscopy by an otolaryngologist to assess mucosal changes and drainage pathways
Sinus Headache Treatment and Management
Pharmacological Therapy
For Acute Bacterial Sinusitis:
- Antibiotics (e.g., amoxicillin-clavulanate)
- Nasal corticosteroids (fluticasone, mometasone)
- Decongestants (pseudoephedrine orally or oxymetazoline topically, limited to 3–5 days)
- Analgesics (acetaminophen, NSAIDs)
For Allergic Causes:
- Antihistamines (loratadine, cetirizine)
- Allergen avoidance
- Immunotherapy in refractory cases
Supportive Measures
- Steam inhalation
- Saline nasal irrigation
- Hydration
- Rest in elevated head position
Interventional and Surgical Options
Balloon Sinuplasty
Minimally invasive procedure that dilates sinus openings to restore drainage.
Functional Endoscopic Sinus Surgery (FESS)
Indicated for chronic or recurrent sinusitis unresponsive to medical therapy or when structural abnormalities are present.
Preventive Strategies for Sinus Headache
- Treat allergies early and consistently
- Maintain optimal indoor air quality with humidifiers
- Avoid known irritants (smoke, pollution, chemical fumes)
- Practice regular nasal hygiene using saline sprays or neti pots
- Manage underlying chronic rhinosinusitis or deviated septum proactively
When to Seek Medical Attention
Immediate medical evaluation is necessary in the following scenarios:
- Severe headache unresponsive to over-the-counter treatment
- High fever or vision changes
- Neurological symptoms (confusion, stiff neck, focal deficits)
- Swelling around the eyes or forehead
- Suspected complications like orbital cellulitis or abscess
Prognosis
Most sinus headaches resolve with conservative treatment or targeted antibiotics. Chronic cases require multidisciplinary care involving primary physicians, allergists, and ENT specialists. Early diagnosis and adherence to therapy are pivotal in minimizing recurrence and complications.
Sinus headaches result from inflammation and blockage of the sinus cavities, leading to characteristic facial pain and pressure. Distinguishing them from primary headache disorders such as migraines is crucial. Comprehensive management including symptom relief, treatment of underlying causes, and preventive strategies offers significant long-term benefit. We emphasize evidence-based care and vigilant follow-up to ensure patient well-being and symptom resolution.