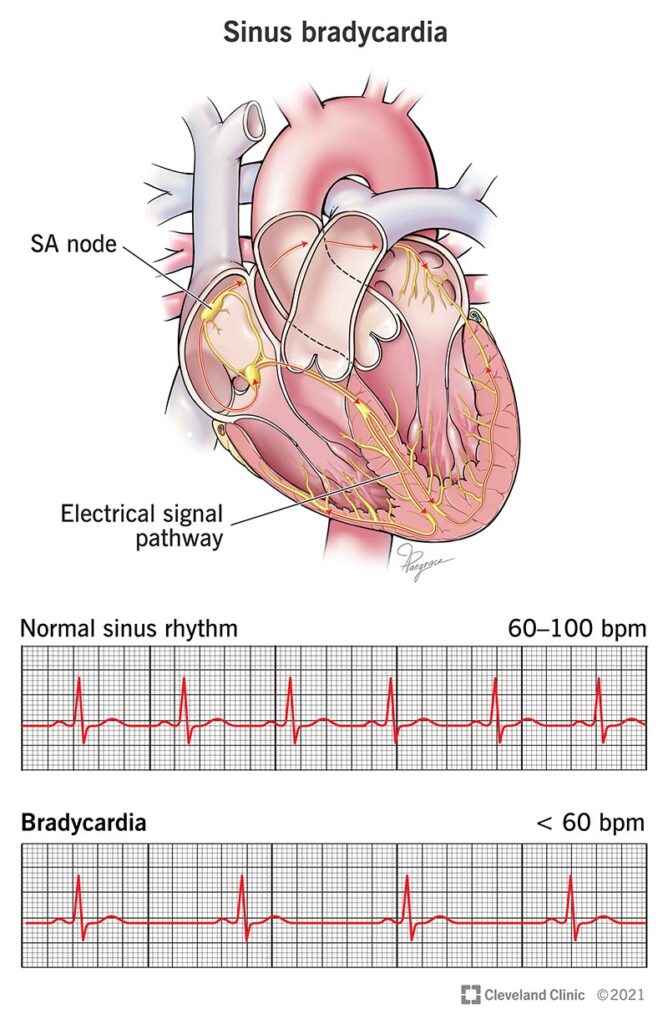
Sinus bradycardia refers to a heart rhythm that originates from the sinoatrial (SA) node but at a rate slower than the normal resting threshold. Defined as a heart rate below 60 beats per minute in adults, this arrhythmia is often benign but can also signify an underlying pathological or physiological process depending on the clinical context.
Physiology of the Sinoatrial Node and Heart Rate Regulation
The SA node, located in the right atrial wall near the superior vena cava, functions as the primary pacemaker of the heart. It generates impulses that propagate through the atria and initiate cardiac contraction.
Autonomic nervous system balance—sympathetic stimulation and parasympathetic (vagal) inhibition—modulates the rate of SA node firing. Enhanced vagal tone or diminished sympathetic activity contributes to sinus bradycardia.
Etiologies of Sinus Bradycardia
Physiological Causes:
- Athletic training (increased vagal tone)
- Sleep (natural nocturnal bradycardia)
- Meditation or deep relaxation states
Pathological Causes:
- Hypothyroidism
- Hypothermia
- Increased intracranial pressure
- Sick sinus syndrome (SA node dysfunction)
- Acute myocardial infarction, particularly inferior wall
- Obstructive sleep apnea
Pharmacologic Causes:
- Beta-blockers
- Calcium channel blockers (non-dihydropyridines)
- Digoxin
- Amiodarone
- Clonidine
Clinical Manifestations of Sinus Bradycardia
Symptoms are often dependent on the rate and patient-specific tolerance. While some patients remain asymptomatic, others may experience:
- Fatigue
- Dizziness or lightheadedness
- Syncope or presyncope
- Shortness of breath
- Exercise intolerance
- Confusion (especially in elderly patients)
In severe cases, inadequate cardiac output may lead to hypotension, heart failure, or cardiogenic shock.
Sinus Bradycardia on Electrocardiogram (ECG)
ECG Characteristics:
- Regular rhythm
- Rate < 60 bpm
- Normal P wave morphology and axis
- Consistent PR intervals
- Normal QRS complexes
Diagnosis is confirmed by correlating clinical signs with ECG findings. A Holter monitor or event recorder may be necessary in intermittent cases.
Evaluation and Diagnostic Workup
Initial Assessment:
- Detailed history including medication use and comorbidities
- Physical examination for signs of hemodynamic compromise
- 12-lead ECG
- Blood tests: TSH, electrolytes, cardiac enzymes (if MI suspected)
Advanced Evaluation:
- Echocardiography to assess cardiac structure and function
- Exercise stress test for chronotropic incompetence
- Electrophysiologic studies in select cases
Treatment of Sinus Bradycardia
Asymptomatic Bradycardia:
No intervention is typically required. Regular monitoring is sufficient.
Symptomatic Bradycardia:
Management depends on urgency and underlying cause.
Acute Management:
- Atropine 0.5 mg IV, repeated every 3–5 minutes up to 3 mg
- If ineffective:
- Transcutaneous pacing
- Dopamine or epinephrine infusion
Long-Term Management:
- Permanent pacemaker implantation in patients with:
- Sinus node dysfunction and symptoms
- Chronotropic incompetence
- Pause-dependent syncope
Medication Review:
Discontinuation or dose adjustment of heart rate-lowering drugs is crucial.
Special Considerations
Sinus Bradycardia in Athletes:
Well-trained individuals may have resting heart rates as low as 30–40 bpm without adverse symptoms. No treatment is required unless symptomatic.
Pediatric Bradycardia:
Heart rate thresholds vary by age. Bradycardia in children may signify hypoxia, especially in neonates and infants.
Bradycardia in Acute MI:
Occurs more frequently in inferior wall infarction due to enhanced vagal tone or AV nodal ischemia. Usually transient but may require pacing.
Complications Associated with Sinus Bradycardia
- Syncope-related trauma
- Decreased cerebral perfusion
- Heart failure exacerbation
- Sudden cardiac arrest (rare)
- Chronotropic incompetence affecting exercise tolerance
Prognosis
When due to reversible or physiological causes, the prognosis is excellent. In cases of structural sinus node disease or conduction abnormalities, the requirement for a pacemaker increases, but outcomes improve significantly with appropriate management.
Preventive and Monitoring Strategies
- Regular cardiac checkups in elderly or high-risk patients
- Routine ECGs when starting rate-lowering medications
- Monitoring athletes with bradycardia and reduced exercise tolerance
- Holter monitoring for intermittent symptoms
Sinus bradycardia, while often benign, must be assessed in clinical context to distinguish physiologic adaptation from pathologic dysfunction. Accurate ECG interpretation, thorough clinical evaluation, and judicious use of pacing therapies or pharmacologic agents ensure optimal patient outcomes. We emphasize early detection and individualized management to prevent complications and maintain cardiovascular stability.