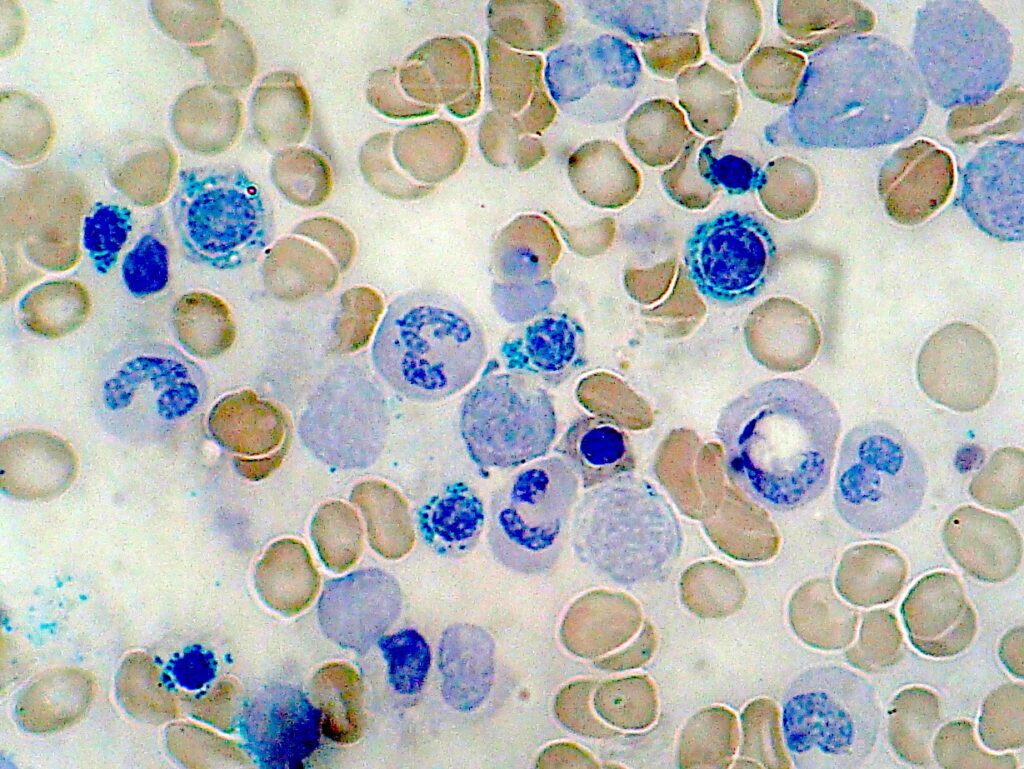
Sideroblastic anemia is a heterogeneous group of blood disorders characterized by the bone marrow’s inability to properly incorporate iron into hemoglobin despite adequate or increased iron stores. This results in the accumulation of iron within the mitochondria of erythroid precursors, forming ring sideroblasts—a hallmark feature identifiable through bone marrow examination.
Pathophysiology: The Mechanism of Iron Dysregulation
At the cellular level, sideroblastic anemia arises from defective heme biosynthesis or iron-sulfur cluster formation within mitochondria. In affected erythroid precursors, iron is transported into mitochondria but fails to be incorporated into heme, leading to toxic mitochondrial iron overload and ineffective erythropoiesis.
Classification of Sideroblastic Anemia
1. Congenital Sideroblastic Anemia (CSA)
Key Subtypes:
- X-linked Sideroblastic Anemia (XLSA): Caused by mutations in the ALAS2 gene affecting δ-aminolevulinic acid synthase 2.
- Autosomal Recessive Forms: Associated with SLC25A38, GLRX5, and other genes involved in iron metabolism or mitochondrial function.
Clinical Features:
- Onset during infancy or early childhood
- Microcytic or normocytic anemia
- Systemic iron overload due to ineffective erythropoiesis
2. Acquired Sideroblastic Anemia
Subtypes:
- Primary (Clonal): Often linked to myelodysplastic syndromes (MDS), particularly MDS with ring sideroblasts (MDS-RS).
- Secondary: Caused by external factors including:
- Chronic alcohol use
- Lead poisoning
- Vitamin B6 (pyridoxine) deficiency
- Copper deficiency
- Certain drugs (e.g., isoniazid, chloramphenicol, linezolid)
Clinical Presentation: Recognizing Symptoms and Signs
Patients with sideroblastic anemia may present with:
- Fatigue, pallor, and weakness
- Exertional dyspnea
- Tachycardia
- Hepatosplenomegaly (in iron overload cases)
- Bronze skin (in severe iron accumulation)
- Neurological symptoms in cases of lead poisoning or vitamin deficiencies
Diagnostic Evaluation
1. Laboratory Investigations
- Complete Blood Count (CBC):
- Typically shows microcytic or normocytic anemia
- Elevated red cell distribution width (RDW)
- Peripheral Blood Smear:
- Hypochromic, microcytic RBCs
- Basophilic stippling in lead poisoning
- Iron Studies:
- Elevated serum ferritin
- Increased transferrin saturation
- Low or normal total iron-binding capacity (TIBC)
2. Bone Marrow Examination
- Key to definitive diagnosis
- Ring sideroblasts: Erythroid precursors with perinuclear iron-laden mitochondria visible with Prussian blue stain
3. Molecular and Genetic Testing
- Identification of mutations in ALAS2, SLC25A38, or SF3B1 gene (especially in MDS-RS)
- Next-generation sequencing panels assist in precise subtyping
Treatment and Management Strategies
1. Pyridoxine (Vitamin B6) Therapy
- First-line treatment in X-linked sideroblastic anemia
- 50–200 mg/day may lead to hematologic response
2. Management of Iron Overload
- Iron chelation therapy (e.g., deferoxamine, deferasirox) in patients with transfusion dependency or significant iron excess
3. Addressing Secondary Causes
- Cessation of offending drugs
- Alcohol abstinence
- Lead chelation in confirmed cases
- Nutritional supplementation for copper or B6 deficiencies
4. Erythropoiesis-Stimulating Agents (ESAs)
- Used in MDS-related sideroblastic anemia with low endogenous erythropoietin levels
5. Luspatercept Therapy
- Recently approved for MDS with ring sideroblasts
- Enhances late-stage erythroid maturation
6. Allogeneic Stem Cell Transplant
- Considered in severe congenital or MDS-associated cases with progression to high-risk disease
Complications and Prognosis
Uncontrolled sideroblastic anemia, particularly in transfusion-dependent individuals, leads to:
- Iron overload with cardiac, hepatic, and endocrine complications
- Risk of transformation to acute myeloid leukemia (AML) in clonal forms
- Progressive marrow failure in untreated congenital forms
Prognostic Factors:
- Age of onset
- Responsiveness to pyridoxine
- Cytogenetic abnormalities in MDS
- Iron burden management
Preventive Measures and Monitoring
- Regular serum ferritin and transferrin saturation monitoring
- Periodic liver MRI for non-invasive iron quantification
- Annual bone marrow assessments in clonal disease
- Genetic counseling for families affected by congenital sideroblastic anemia
Sideroblastic anemia encompasses a diverse group of disorders unified by ineffective erythropoiesis and mitochondrial iron trapping. Accurate diagnosis through marrow examination, iron studies, and molecular testing is vital for appropriate classification and treatment. With targeted interventions, including pyridoxine therapy and iron chelation, many patients can achieve hematologic stability and improved quality of life.