Sialorrhea, commonly known as excessive drooling, refers to the unintentional loss of saliva from the mouth. It results either from hypersalivation or from impaired oral motor control, often associated with neurological conditions. Sialorrhea significantly impacts quality of life, affecting speech, swallowing, social interaction, and increasing the risk of aspiration.
Types of Sialorrhea
Sialorrhea can be classified based on etiology and duration:
- Anterior Sialorrhea – Drooling from the mouth, typically visible.
- Posterior Sialorrhea – Saliva pooling in the oropharynx, posing a risk for aspiration.
Chronic vs. Acute Sialorrhea
- Chronic sialorrhea is commonly associated with neurodevelopmental or neurodegenerative disorders.
- Acute sialorrhea may arise due to medication side effects or oral infections.
Pathophysiology of Sialorrhea
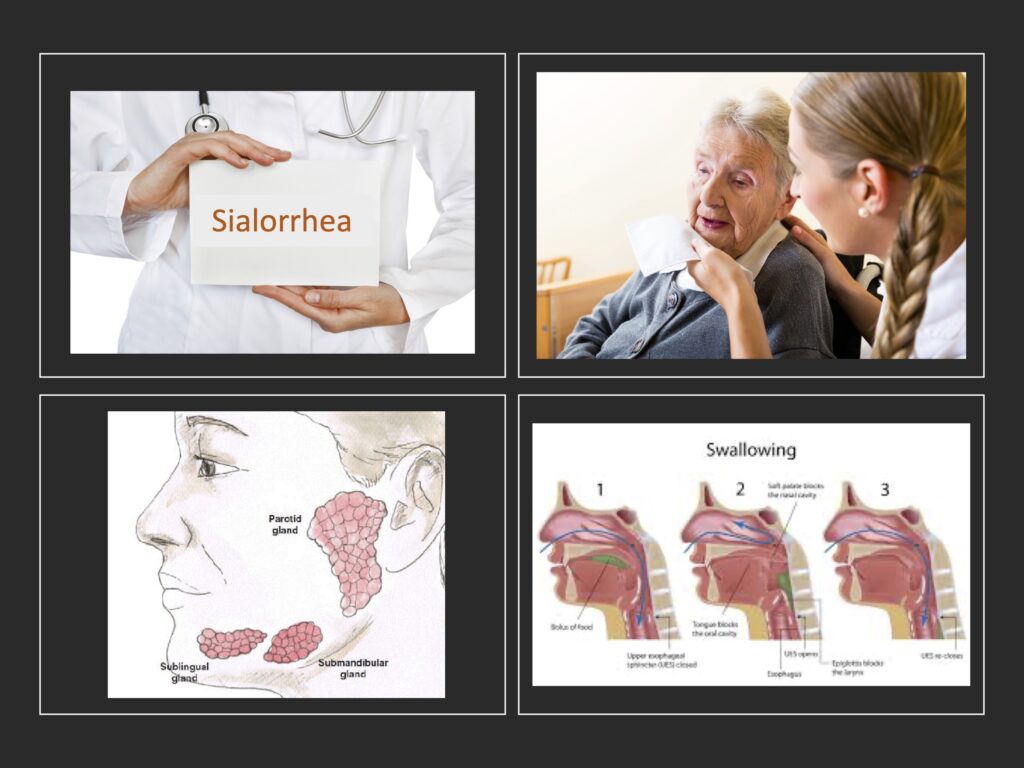
Saliva is secreted by three major salivary glands: parotid, submandibular, and sublingual. While normal adults produce 1 to 1.5 liters daily, most of it is swallowed unconsciously. Impairment in salivary control mechanisms—either increased production or impaired clearance—leads to drooling.
Common Causes of Sialorrhea
Neurological Disorders
- Cerebral palsy
- Parkinson’s disease
- Amyotrophic lateral sclerosis (ALS)
- Stroke
- Traumatic brain injury
These conditions impair motor control of facial and oral muscles, leading to inefficient swallowing and drooling.
Medications
- Cholinergic agents (e.g., clozapine)
- Antipsychotics
- Anticonvulsants
Structural or Functional Abnormalities
- Enlarged tonsils or adenoids
- Malocclusion
- Oral infections
- Nasal obstructions
Developmental Factors in Children
Infants and toddlers may have transient sialorrhea during teething or due to immature neuromuscular control, usually resolving with age.
Clinical Presentation and Complications
Symptoms
- Constant wetness around the mouth
- Skin maceration and irritation
- Halitosis
- Chapped lips
Psychosocial Effects
- Social embarrassment
- Reduced self-esteem
- Caregiver burden in pediatric or geriatric cases
Medical Risks
- Aspiration pneumonia
- Dehydration
- Feeding difficulties
Diagnostic Approach to Sialorrhea
Diagnosis is primarily clinical, supported by history, physical examination, and severity scales.
Assessment Tools
- Drooling Severity and Frequency Scale (DSFS)
- Teacher Drooling Scale (for children)
- Saliva measurement tests (e.g., bib weight, suction counts)
Key Evaluation Parameters
- Duration and frequency of drooling
- Impact on quality of life
- Underlying neurological or anatomical abnormalities
- Response to prior treatments
Effective Treatment Options for Sialorrhea
1. Conservative and Behavioral Interventions
- Speech and occupational therapy
- Oral-motor exercises
- Swallowing training
- Biofeedback
- Postural adjustments
- Oromotor aids and reminder cues
2. Pharmacologic Management
| Medication | Mechanism | Common Side Effects |
|---|---|---|
| Glycopyrrolate | Anticholinergic | Dry mouth, constipation |
| Scopolamine patches | Anticholinergic (transdermal) | Blurred vision, confusion |
| Atropine eye drops | Sublingual administration | Tachycardia, flushing |
| Botulinum toxin A/B | Inhibits acetylcholine release | Localized muscle weakness |
Botulinum toxin injections into the parotid and submandibular glands offer a minimally invasive, reversible option with effects lasting 3–6 months.
3. Surgical and Interventional Therapies
- Duct ligation or relocation
- Redirecting saliva flow posteriorly for easier swallowing
- Gland excision
- Reserved for refractory pediatric or severe adult cases
- Radiation therapy
- Used in select elderly or palliative care patients
Management Strategies Based on Etiology
| Condition | Preferred Treatment Modalities |
|---|---|
| Cerebral palsy | Oral therapy + botulinum toxin |
| Parkinson’s disease | Anticholinergics, botulinum toxin |
| ALS | Botulinum toxin, radiation (late-stage) |
| Medication-induced | Dose adjustment or substitution |
Pediatric Considerations in Sialorrhea
In children, especially those with cerebral palsy, sialorrhea may persist beyond early development and significantly affect nutrition, hygiene, and communication. Management should be interdisciplinary, involving pediatric neurologists, speech therapists, and ENT specialists.
Goals of Therapy
- Improve swallowing function
- Minimize social stigma
- Prevent complications such as aspiration or dermatitis
Prognosis and Follow-up
Sialorrhea is chronic but manageable. Prognosis depends on the underlying cause and treatment adherence. Long-term follow-up is essential to monitor treatment response and adjust strategies accordingly.
Monitoring Checklist
- Periodic reassessment with DSFS
- Evaluate impact on social, nutritional, and respiratory health
- Titrate pharmacologic therapies to minimize side effects
Sialorrhea is a multifactorial condition with significant physical, emotional, and social consequences. A tailored, multidisciplinary approach that includes behavioral strategies, pharmacologic therapy, and surgical options—where necessary—yields the best outcomes. Early identification and targeted intervention play a pivotal role in enhancing patient comfort and quality of life.