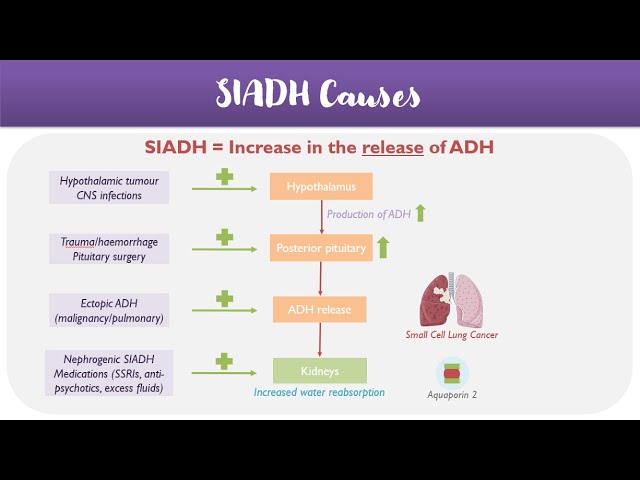
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) is a disorder characterized by excessive release of antidiuretic hormone (ADH), also known as vasopressin. This hormone regulates water retention in the body, and its overproduction leads to water retention and dilutional hyponatremia—low sodium levels in the blood. SIADH is a form of euvolemic hyponatremia, meaning that despite low sodium levels, there is no clinical sign of fluid overload or depletion.
Pathophysiology of SIADH
ADH acts on the renal collecting ducts to promote water reabsorption. In SIADH, ADH is secreted inappropriately despite normal or low plasma osmolality. This leads to excessive water retention, reduced plasma sodium concentration, and decreased serum osmolality. The kidneys continue to excrete sodium, further exacerbating hyponatremia.
Common Causes of SIADH Syndrome
SIADH can be triggered by a variety of conditions that stimulate or mimic ADH secretion:
Neurological Causes
- Head trauma
- Stroke
- Subarachnoid hemorrhage
- Meningitis
- Encephalitis
Pulmonary Disorders
- Pneumonia
- Tuberculosis
- Acute respiratory failure
- Positive pressure ventilation
Malignancies
- Small-cell lung carcinoma (most common)
- Pancreatic cancer
- Prostate cancer
- Lymphomas and leukemias
Medications
- SSRIs (e.g., fluoxetine)
- Antipsychotics (e.g., haloperidol)
- Antiepileptics (e.g., carbamazepine)
- Chemotherapy agents (e.g., vincristine)
- NSAIDs and opioids
Others
- Postoperative state
- Pain or nausea
- Idiopathic in elderly individuals
Clinical Symptoms of SIADH Syndrome
Symptoms vary depending on the severity and rapidity of onset of hyponatremia:
Mild to Moderate Hyponatremia (Na+ 125–134 mmol/L)
- Fatigue
- Headache
- Nausea
- Anorexia
- Muscle cramps
Severe Hyponatremia (Na+ <125 mmol/L)
- Vomiting
- Confusion
- Seizures
- Coma
- Respiratory arrest
Chronic hyponatremia may present with subtle cognitive and gait disturbances, especially in older adults.
Diagnostic Criteria for SIADH
Diagnosis is clinical and based on laboratory findings after ruling out other causes of hyponatremia.
Key Diagnostic Findings:
- Serum sodium <135 mmol/L
- Serum osmolality <275 mOsm/kg
- Urine osmolality >100 mOsm/kg
- Urine sodium >40 mmol/L (with normal salt intake)
- Euvolemic status (no signs of fluid overload or depletion)
- Normal renal, adrenal, and thyroid function
Differential Diagnosis
Before confirming SIADH, it is essential to exclude other potential causes of hyponatremia, including:
- Hypovolemic hyponatremia (e.g., due to vomiting, diarrhea)
- Hypervolemic hyponatremia (e.g., in CHF, cirrhosis, nephrotic syndrome)
- Endocrinopathies (e.g., hypothyroidism, adrenal insufficiency)
Treatment of SIADH Syndrome
Initial Management:
- Fluid Restriction: First-line approach (typically 800–1000 mL/day)
- Discontinuation of causative drugs
- Addressing the underlying cause (e.g., treating infections or malignancies)
Moderate to Severe Cases:
- Hypertonic Saline (3% NaCl): Administer cautiously in acute or symptomatic hyponatremia.
- Loop Diuretics: Used with saline to promote free water excretion.
- Oral Salt Tablets: For chronic SIADH.
Vasopressin Receptor Antagonists (Vaptans):
- Tolvaptan or Conivaptan selectively block V2 receptors to promote aquaresis.
- Used in hospitalized patients under close monitoring.
Important Consideration:
- Avoid rapid correction of sodium to prevent osmotic demyelination syndrome (ODS).
- Maximum correction rate: 8–10 mmol/L in 24 hours
Prognosis and Monitoring
The prognosis of SIADH depends on the underlying cause and the promptness of intervention. Recurrent or persistent cases require long-term management and patient education. Routine monitoring of serum sodium, urine osmolality, and adherence to fluid restrictions is vital.
SIADH in Special Populations
Elderly
- More susceptible due to increased sensitivity to ADH and frequent use of medications like SSRIs and diuretics.
Postoperative Patients
- Stress response and narcotics increase ADH secretion.
Cancer Patients
- Often associated with ectopic ADH production, especially in small-cell lung cancer.
When to Refer
Referral to an endocrinologist or nephrologist is recommended in cases of:
- Severe or recurrent hyponatremia
- Diagnostic uncertainty
- Need for vaptan therapy
- Complications due to rapid correction
SIADH is a significant but treatable cause of hyponatremia. Prompt recognition, appropriate fluid management, identification of the underlying etiology, and careful correction of sodium levels are key to improving patient outcomes. Awareness of potential complications and long-term management strategies ensures optimal care for affected individuals.